Top 8 Alternatives to Prelone in 2024 for Effective Inflammation Relief
October 20 2024Revolving Door in Pharmacy: How Systems Fail and How to Fix Them
When we talk about the revolving door, a pattern where the same mistakes keep happening despite repeated fixes. Also known as cyclical failure, it’s what happens when safety systems look good on paper but don’t work in real life. In pharmacies, this isn’t just a metaphor—it’s a daily reality. A patient gets the wrong dose because a label was misread. A generic drug gets switched without proper monitoring, and blood levels swing dangerously. A manufacturer passes inspection one month, then fails the next because nothing actually changed. These aren’t isolated blunders. They’re symptoms of a system that spins but never moves forward.
The medication errors, preventable mistakes in prescribing, dispensing, or taking drugs. Also known as drug errors, it’s the most visible sign of this revolving door. Studies show hospital pharmacies miss 1 in every 200 doses. Retail pharmacies miss 1 in every 500. Neither number is acceptable. But here’s the twist: when you fix one error, another pops up. Why? Because we fix symptoms, not systems. We add double checks for insulin, but ignore how rushed pharmacists are. We train staff on dangerous abbreviations like "QD" or "MS," but don’t change the software that lets them type it. The drug supply chain, the network of manufacturers, distributors, and pharmacies that deliver medications to patients. Also known as pharmaceutical distribution, it’s another loop that spins without stopping. The DSCSA track-and-trace system was supposed to stop counterfeit drugs. It helps—but only if every link in the chain follows the rules. And too often, they don’t. Quality assurance checks get skipped. Documentation is rushed. Inspections are scheduled, not random. The system expects people to be perfect, but people are fallible. And when you design a system that depends on perfection, you’re already losing.
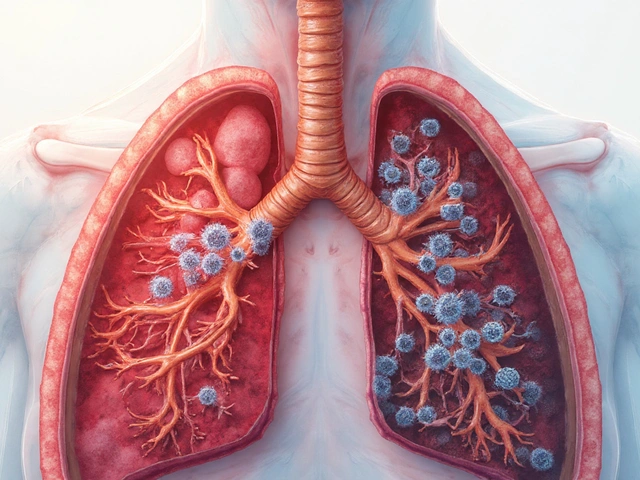
The same pattern shows up in how we treat generics. Patients feel worse after switching—even when the chemistry is identical. Why? Because the healthcare systems, the organized structures that deliver care, including pharmacies, insurers, and regulatory agencies. Also known as medical infrastructure, they treat medication as a commodity, not a life-sustaining tool. They push cost savings over patient trust. They approve generics based on bioequivalence studies that ignore real-world variability. They don’t train providers to explain why a switch might feel different. So patients stop taking their meds. Or worse—they assume the new pill isn’t working and ask for a brand-name replacement. The revolving door spins again.
What’s the fix? Not more rules. Not more training. Not another audit. The fix is designing systems that assume mistakes will happen—and building in ways to catch them before they hurt someone. That means automated alerts that block dangerous combinations. That means labeling that’s clear even under stress. That means inspections that are unannounced and random. That means listening to the pharmacist who says, "This doesn’t feel right." The revolving door won’t stop until we stop pretending it’s the person’s fault—and start fixing the machine.
Below, you’ll find real stories from inside this broken system: how a single abbreviation caused a deadly error, why generic switches can be risky, how inspections miss the real problems, and what’s being done to close the loop for good.
 2 Dec
2 Dec
Regulatory Capture: How Industry Influence Undermines Public Protection
Regulatory capture occurs when government agencies meant to protect the public end up serving the industries they regulate. From the revolving door to hidden lobbying, this systemic problem undermines safety, fairness, and democracy.
Read More...