Not all beta-blockers are the same. Even though they all block adrenaline, the differences between them can mean the difference between feeling better and feeling worse. If you’ve been prescribed a beta-blocker, you might wonder why your doctor chose one over another. Is it just brand names? Price? Or is there something deeper? The truth is, these drugs vary in how they work, what side effects they cause, and who they’re safest for. Choosing the right one isn’t random-it’s based on your heart, your lungs, your age, and even your sex life.
What Beta-Blockers Actually Do
Beta-blockers stop adrenaline from overworking your heart. Adrenaline is your body’s natural stress signal. When it binds to beta receptors, your heart beats faster, harder, and your blood pressure rises. That’s useful if you’re running from a bear. Not so useful if you’re sitting at your desk with high blood pressure or recovering from a heart attack.
By blocking those receptors, beta-blockers slow your heart rate, lower blood pressure, and reduce how hard your heart pumps. That’s why they’re used after heart attacks, for heart failure, irregular rhythms, and even migraines. But here’s the catch: not all beta receptors are the same. There are three types-β1, β2, and β3-and different drugs target them differently. That’s where the real differences begin.
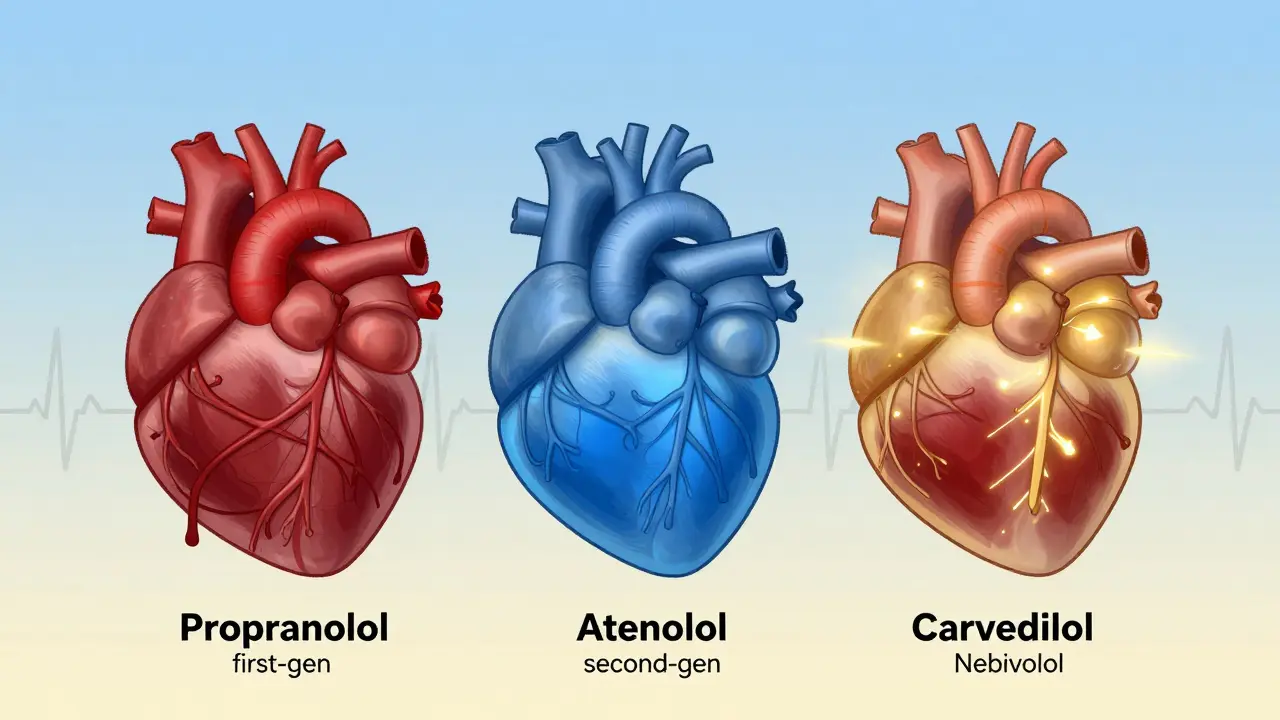
The Three Generations of Beta-Blockers
There are three clear generations of beta-blockers, each with distinct traits. First-generation drugs like propranolol block all beta receptors-β1 and β2. That means they affect your heart, your lungs, your blood vessels, and even your metabolism. That broad action makes them powerful, but also riskier. People with asthma or COPD can have serious breathing problems on these drugs because β2 receptors in the airways get blocked too.
Second-generation beta-blockers like atenolol, metoprolol, and bisoprolol are more selective. They mostly target β1 receptors in the heart. That’s why they’re called cardioselective. They still lower heart rate and blood pressure, but they’re less likely to cause wheezing or cold hands. This makes them safer for people with lung issues-but not risk-free. Even cardioselective drugs can affect the lungs at high doses.
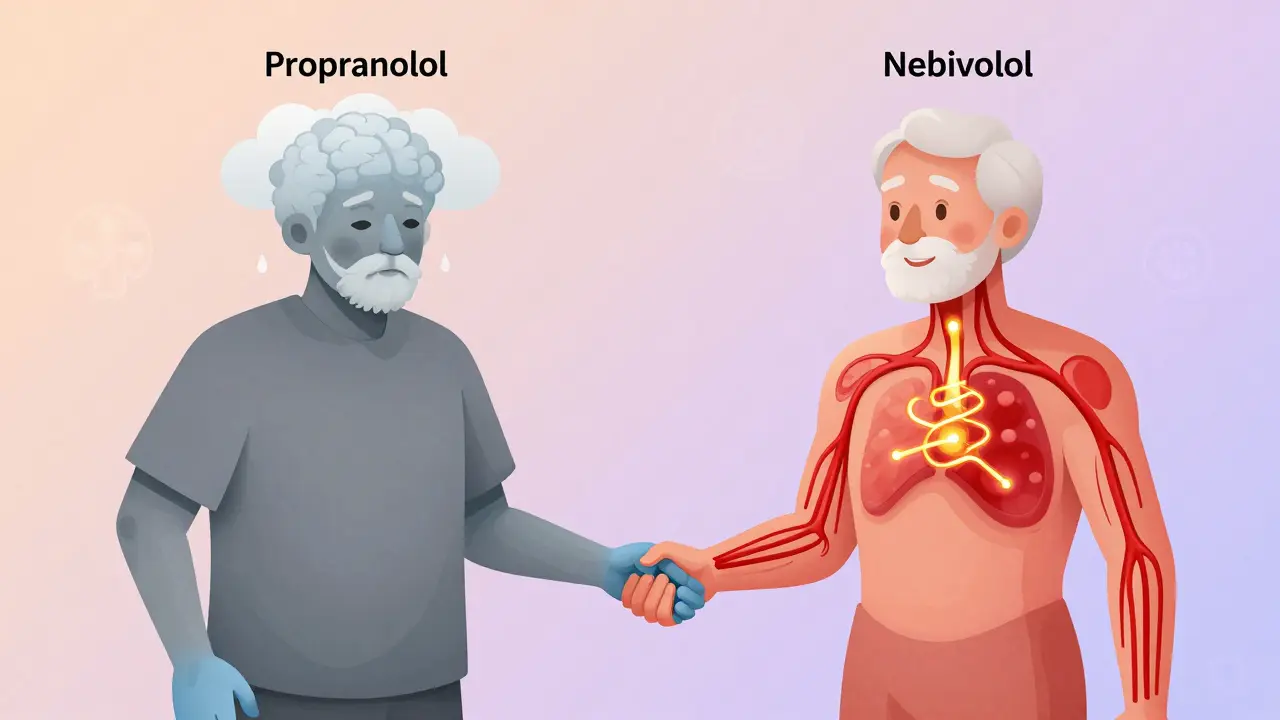
Third-generation drugs like carvedilol and nebivolol go further. They don’t just block beta receptors-they also widen blood vessels. Carvedilol blocks α1 receptors, which relaxes arteries. Nebivolol triggers nitric oxide release, which does the same thing. This extra vasodilation means better blood flow, less strain on the heart, and fewer side effects like fatigue. These are the drugs now recommended for heart failure because they don’t just slow the heart-they help it heal.
Why Carvedilol and Nebivolol Stand Out in Heart Failure
If you have heart failure with reduced pumping ability, your doctor will likely choose carvedilol or nebivolol over older options. Why? Because they don’t just manage symptoms-they improve survival.
In the US Carvedilol Heart Failure Study from 1996, patients on carvedilol had a 35% lower risk of dying compared to those on placebo. Nebivolol, in the SENIORS trial, cut cardiovascular deaths by 14% in older adults. These aren’t small numbers. They’re life-changing.
Carvedilol also fights oxidative stress in heart tissue. Preclinical studies show it reduces damaging free radicals by 30-40%, something traditional beta-blockers don’t do. Nebivolol improves blood vessel function, reduces fibrosis, and even protects heart cells from dying. These aren’t side effects-they’re therapeutic benefits built into the drug’s design.
That’s why the European Society of Cardiology recommends these two as first-line choices for heart failure. They’re not just alternatives-they’re upgrades.
Side Effects: Not All Beta-Blockers Are Created Equal
Everyone hears about beta-blocker side effects: fatigue, cold hands, low energy. But some drugs cause these more than others.
Propranolol, the original, has the worst reputation. Patient reviews on Drugs.com show 38% report moderate to severe side effects-sleep problems, depression, trouble exercising. It crosses the blood-brain barrier easily, which may explain why it’s linked to mood changes.
Compare that to bisoprolol. Its average rating is 7.1 out of 10. Only 18% report sleep issues, and 11% feel depressed. Why? It doesn’t cross into the brain as much. That makes it a better fit for people who need heart protection without mental fog.
Then there’s nebivolol. Men over 50 on Reddit’s r/Cardiology report better sexual function on nebivolol than on older beta-blockers. Why? Because it boosts nitric oxide, which improves blood flow-not just to the heart, but everywhere. Traditional beta-blockers can cause erectile dysfunction by reducing blood flow. Nebivolol might actually help.
And cold hands? That’s mostly from β2 blockade. Nonselective drugs like propranolol cause it in 29% of users. Cardioselective ones like metoprolol? Around 15%. Nebivolol? Even less, thanks to its vasodilating effect.
Dosing and Practical Differences
It’s not just about what the drug does-it’s about how you take it.
Metoprolol comes in two forms: tartrate (Lopressor) and succinate (Toprol XL). Tartrate needs to be taken twice a day. Succinate is once daily. That matters for adherence. If you forget a pill, your heart rate can spike. Extended-release versions smooth that out.
Carvedilol requires slow titration. You start at 3.125 mg twice daily and increase slowly over 8-16 weeks. Jumping to the full dose can cause dizziness or low blood pressure. Bisoprolol? You can ramp up faster-over 4-8 weeks. That’s easier for patients and doctors alike.
And don’t forget the paperwork. Nebivolol’s FDA label is 47 pages long. Propranolol’s is 28. Why? Nebivolol has more complex data-more trials, more endpoints, more safety details. That’s because it’s newer, and regulators expect more proof.
Who Should Avoid Which Beta-Blocker?
Here’s a quick guide to avoid trouble:
- Asthma or COPD? Avoid propranolol and labetalol. Stick with cardioselective agents like bisoprolol or metoprolol, but still monitor closely.
- Diabetes? Beta-blockers can mask low blood sugar symptoms (like a fast heartbeat). Carvedilol and nebivolol are preferred because they’re less likely to interfere with glucose recovery.
- Depression or fatigue? Skip propranolol. Try bisoprolol or nebivolol-they’re gentler on the mind.
- Erectile dysfunction? Nebivolol may help. Others might make it worse.
- Over 80? Be careful. One study found 28% of prescriptions in elderly patients were inappropriate. Avoid high doses unless clearly needed.
Why Beta-Blockers Are No Longer First-Line for High Blood Pressure
You might be surprised: beta-blockers aren’t the go-to for simple high blood pressure anymore. Why? Because they don’t lower central aortic pressure as well as ACE inhibitors or calcium channel blockers. They reduce heart rate and output, but they don’t relax arteries as effectively. That means less protection against stroke and kidney damage.
According to the Mayo Clinic’s 2023 update, beta-blockers are now reserved for hypertension only when there’s another reason to use them-like a prior heart attack, heart failure, or fast heart rhythm. For pure high blood pressure without heart disease, other drugs work better and cause fewer side effects.
What’s Next for Beta-Blockers?
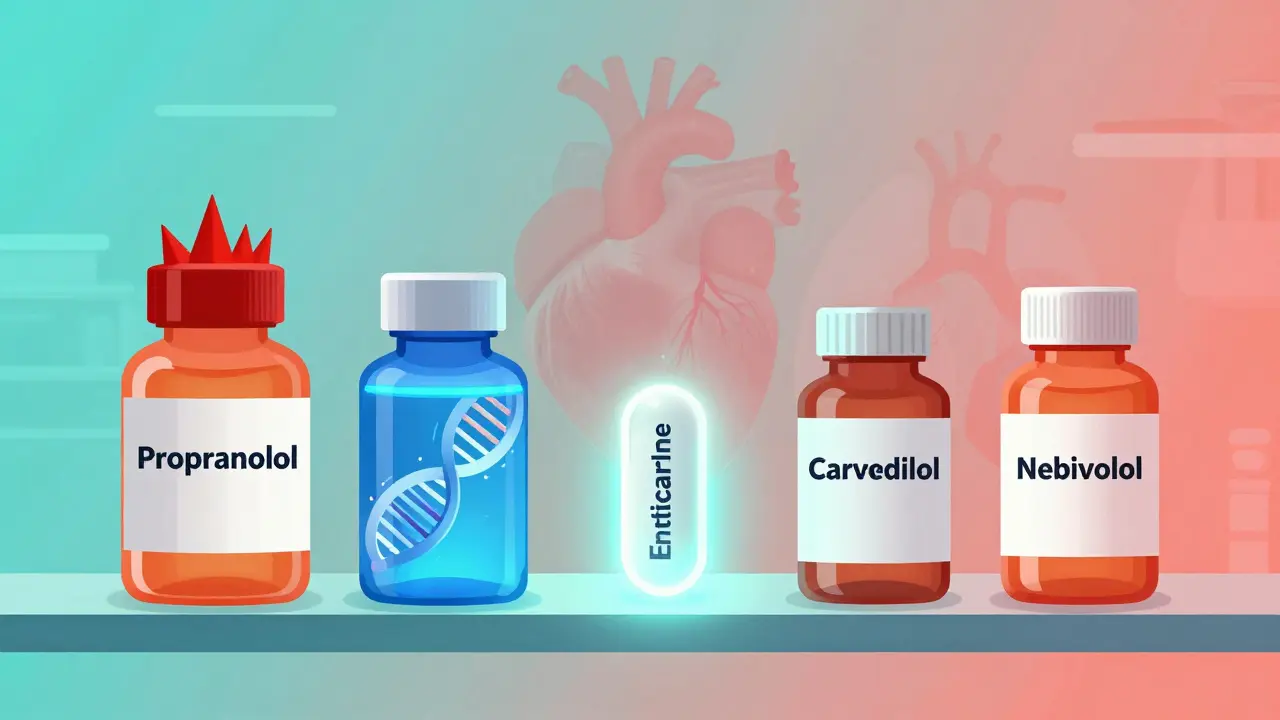
The field isn’t standing still. In 2023, the FDA approved a new drug-entricarone-that combines a beta-3 agonist with beta-1 blockade. Early trials show it cuts heart failure hospitalizations by 22% in patients with preserved ejection fraction, a group that’s been hard to treat.
Next up: nebivolol combined with valsartan (an ARB) in one pill, expected in 2024. That could simplify treatment for people with both high blood pressure and heart failure.
And researchers are testing gene-based selection. The GENETIC-BB trial is looking at whether your DNA can predict which beta-blocker you’ll respond to best. Imagine a simple blood test telling you: “You’ll do better on nebivolol than metoprolol.” That’s the future.
Final Takeaway: It’s Not One Size Fits All
Beta-blockers are not interchangeable. Propranolol isn’t just an older version of carvedilol-it’s a different tool. The right choice depends on your condition, your other health issues, your age, and even your quality of life. A drug that helps your heart might hurt your sleep. One that lowers your blood pressure might help your sex life. Your doctor’s job isn’t to pick the cheapest or the newest-it’s to pick the one that works for you.
If you’re on a beta-blocker and not feeling well, don’t just assume it’s normal. Ask: Is this the right one? Could another version work better? The answer could change how you feel every day.
Are all beta-blockers the same?
No. Beta-blockers vary by generation, selectivity, and additional effects. First-generation drugs like propranolol block all beta receptors and can cause breathing issues. Second-generation drugs like metoprolol are heart-selective. Third-generation drugs like carvedilol and nebivolol also widen blood vessels, offering extra heart protection and fewer side effects.
Which beta-blocker is best for heart failure?
Carvedilol and nebivolol are preferred for heart failure with reduced ejection fraction. Both have been shown in large trials to reduce death rates. Carvedilol lowers oxidative stress, while nebivolol improves blood vessel function. Bisoprolol is also recommended. Older drugs like atenolol are not first-line for this condition.
Can beta-blockers cause depression or fatigue?
Yes, especially propranolol, because it crosses into the brain. Studies show 19-27% of users report depression or sleep issues. Drugs like bisoprolol and nebivolol are less likely to cause these because they don’t enter the brain as easily. If you’re feeling tired or low, talk to your doctor about switching.
Why are beta-blockers no longer first-line for high blood pressure?
Because they don’t lower central aortic pressure as effectively as other drugs like ACE inhibitors or calcium channel blockers. While they reduce heart rate and output, they don’t relax arteries as well. For pure high blood pressure without heart disease, other medications offer better protection against stroke and kidney damage with fewer side effects.
Is it safe to stop beta-blockers suddenly?
No. Stopping abruptly can trigger a rebound surge in adrenaline, raising your heart rate and blood pressure sharply. This increases the risk of heart attack by up to 300% in the first 48 hours. Always taper off under medical supervision-even if you feel fine.
Do beta-blockers affect sexual function?
Many older beta-blockers like propranolol and metoprolol can cause erectile dysfunction by reducing blood flow. Nebivolol is different-it improves blood flow by boosting nitric oxide. Studies show men on nebivolol report better sexual function compared to those on other beta-blockers.





Emily P
December 21, 2025 AT 01:32