The Role of Atomoxetine in End-of-Life Care
July 21 2023Lp(a) Treatment: What Works, What Doesn't, and What You Need to Know
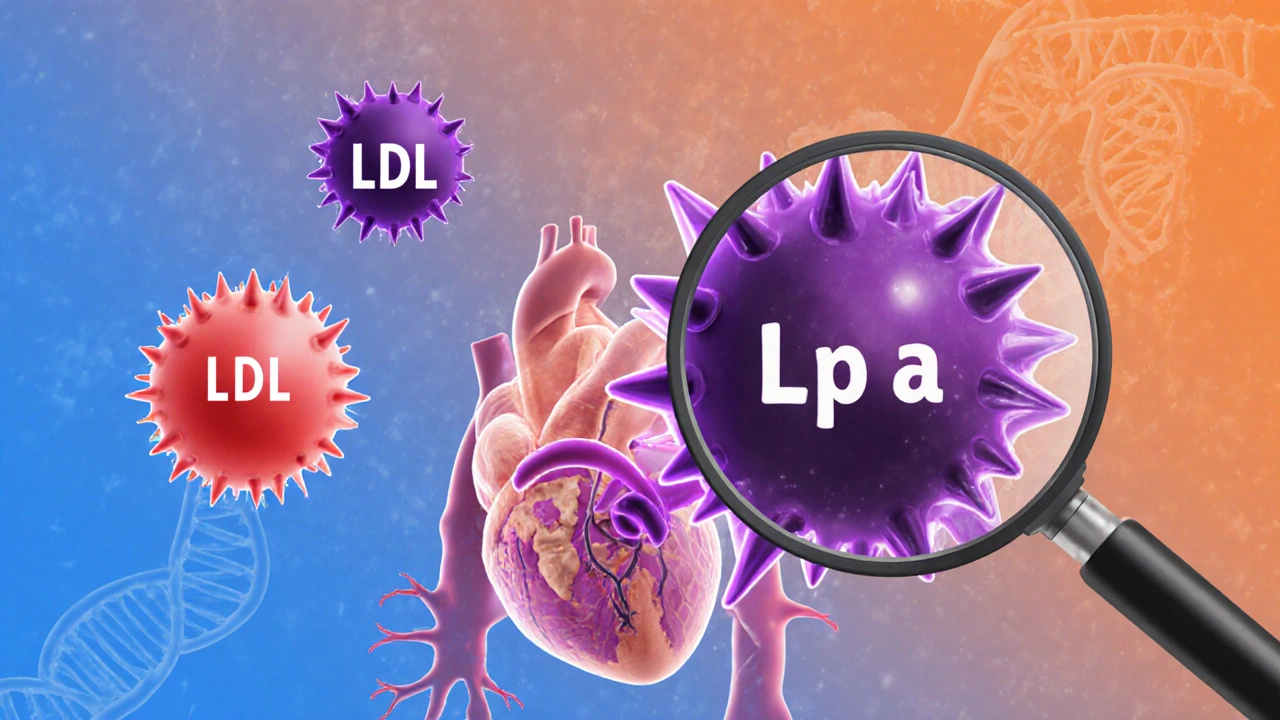
When your doctor says your Lp(a), a type of lipoprotein that carries cholesterol in the blood and is strongly linked to heart disease risk. Also known as lipoprotein(a), it's not something you can fix with diet or exercise alone. is high, it’s not a mistake—it’s a genetic red flag. Unlike LDL cholesterol, which drops with statins and lifestyle changes, Lp(a) stays stubbornly high in most people. It’s like having a hidden timer ticking inside your arteries, and the higher it is, the greater your chance of a heart attack or stroke, even if everything else looks fine.
That’s why PCSK9 inhibitors, a class of injectable drugs that lower both LDL and Lp(a) by blocking a protein that limits the liver’s ability to remove cholesterol are becoming the go-to for people with elevated Lp(a). Drugs like evolocumab and alirocumab can slash Lp(a) by 20% to 30%, and in some cases even more. That’s not a cure, but it’s one of the few tools we have that actually moves the needle. Meanwhile, statins, common cholesterol-lowering pills like atorvastatin and rosuvastatin may help with your overall heart risk, but they won’t touch Lp(a)—and in some cases, they might even nudge it higher. That’s why simply taking a statin isn’t enough if your Lp(a) is in the danger zone.
There’s no magic pill yet, but new treatments are coming fast. Nucleic acid therapies like pelacarsen are in late-stage trials and show promise in lowering Lp(a) by over 80%. These aren’t available yet, but they’re the future. Right now, your best move is knowing your number, managing everything else you can—blood pressure, smoking, diabetes—and talking to your doctor about whether a PCSK9 inhibitor makes sense. Don’t wait for symptoms. Lp(a) doesn’t cause pain. It just quietly builds plaque until something breaks.
The posts below cover everything you need to connect the dots: from how Lp(a) compares to other cholesterol types, to what drugs actually work (and which ones don’t), to how it ties into heart valve disease, blood thinners, and immune-related conditions like uveitis—all of which can overlap in high-risk patients. You’ll find real-world insights on managing this silent threat, not just textbook definitions. This isn’t about guessing. It’s about knowing what to ask for, what to track, and how to protect your heart before it’s too late.
 20 Nov
20 Nov
Lipoprotein(a): Understanding Your Genetic Heart Risk and What You Can Do
Lipoprotein(a) is a genetic risk factor for heart disease that's often missed in routine checkups. Learn what it is, who's at risk, and what treatments are on the horizon.
Read More...