Generic Drug Contamination: Recent Cases and Prevention Strategies
February 5 2026Brand Consistency: Why Trust in Medications Depends on More Than Just the Name
When you pick up a bottle of brand consistency, the reliable match between how a medication looks, feels, and performs across batches and manufacturers. Also known as pharmaceutical identity, it's what tells you that the blue pill you got last month is the same one you're holding today—even if the label changed or the pharmacy switched suppliers. This isn’t just about marketing. It’s about your body recognizing the medicine it’s been relying on. When brand consistency breaks down—when the shape changes, the color shifts, or the pill tastes different—it triggers doubt. And doubt, in medicine, can mean skipped doses, panic, or worse.
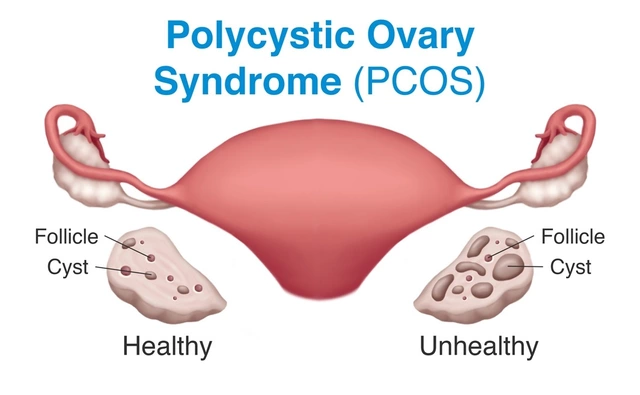
That’s why generic drugs, medications that contain the same active ingredient as brand-name versions but may differ in appearance or inactive ingredients. Also known as non-brand medications, it is often the center of this tension. Legally, generics must be bioequivalent. But bioequivalence doesn’t mean identical. A patient taking warfarin for years might feel off when their pharmacy switches from one generic maker to another—even if the chemistry is the same. Why? Because their brain remembers the pill’s look, the way it felt in their hand, the routine. This isn’t irrational—it’s human. Studies show that medication trust, the confidence patients have in a drug’s reliability based on past experience and perceived consistency drops sharply when packaging or pill appearance changes unexpectedly. Even doctors admit they prescribe based on familiarity, not just science.
And it’s not just about pills. pharmaceutical quality, the uniform standards applied to manufacturing, testing, and packaging to ensure safety and effectiveness is the backbone of brand consistency. If one batch of a drug has different fillers, or a different coating that changes how fast it dissolves, the effect can be real—especially with narrow therapeutic index drugs like phenytoin or cyclosporine. A small change in absorption can mean a seizure, a clot, or a rejection of a transplanted organ. That’s why some hospitals and pharmacies stick to one generic brand, even if it costs more. They’re not being stubborn—they’re protecting lives.
Meanwhile, brand-name medications, originally developed drugs protected by patents, often with distinctive packaging and consistent appearance still carry a psychological weight. People pay more for them—not always because they work better, but because they feel safer. That feeling isn’t empty. It’s built on years of consistent experience: same color, same size, same side effects, same results. When that pattern breaks, trust erodes. And rebuilding it? That’s harder than any clinical trial.
What you’ll find below are real stories and data-driven insights from patients, pharmacists, and doctors who’ve seen what happens when brand consistency falters. From insurance denials that force switches, to cultural fears about generic pills, to how placebo effects shape whether a drug "works"—this collection isn’t about marketing. It’s about the quiet, daily choices that keep people alive. And how even small changes in a pill’s appearance can ripple through someone’s entire health journey.
 26 Nov
26 Nov
Rare Cases Where Staying on Brand Is Better: Individual Customer Response Analysis
In rare but powerful cases, staying on brand - not switching to generics or trendy messaging - builds deeper trust and stronger customer loyalty. Learn why consistency wins in emotional, crisis, and cultural moments.
Read More...