PCP Prophylaxis Risk Calculator
When Do You Need Antibiotics to Prevent a Deadly Lung Infection?
If you're taking high-dose steroids or other strong immunosuppressants, you might not realize you're at risk for a rare but deadly lung infection called Pneumocystis jirovecii pneumonia, or PCP. It’s not common. But when it hits someone with a weakened immune system, it can kill. About 30 to 50% of people who get PCP without being protected die from it. And here’s the problem: many doctors still don’t agree on who needs protection - even though the rules have been around for decades.
PCP used to be mostly seen in people with advanced HIV. But today, it’s more likely to show up in someone taking prednisone for lupus, cyclophosphamide for vasculitis, or a combo of drugs after a kidney transplant. The infection doesn’t come from being around sick people. It’s a fungus that lives quietly in your lungs, waiting for your immune system to drop low enough to let it grow out of control.
Who’s at Real Risk? It’s Not Just About the Drug Name
Not everyone on immunosuppressants needs prophylaxis. But some do - and missing the warning signs can be deadly. The biggest red flag? Taking prednisone at 20 mg or more per day for four weeks or longer. That’s the clear trigger from the British Columbia Renal Agency and CDC guidelines. But here’s the twist: newer research from 2025 shows cases popping up in people on just 10 mg a day - especially if they’re also on another immunosuppressant like mycophenolate or azathioprine.
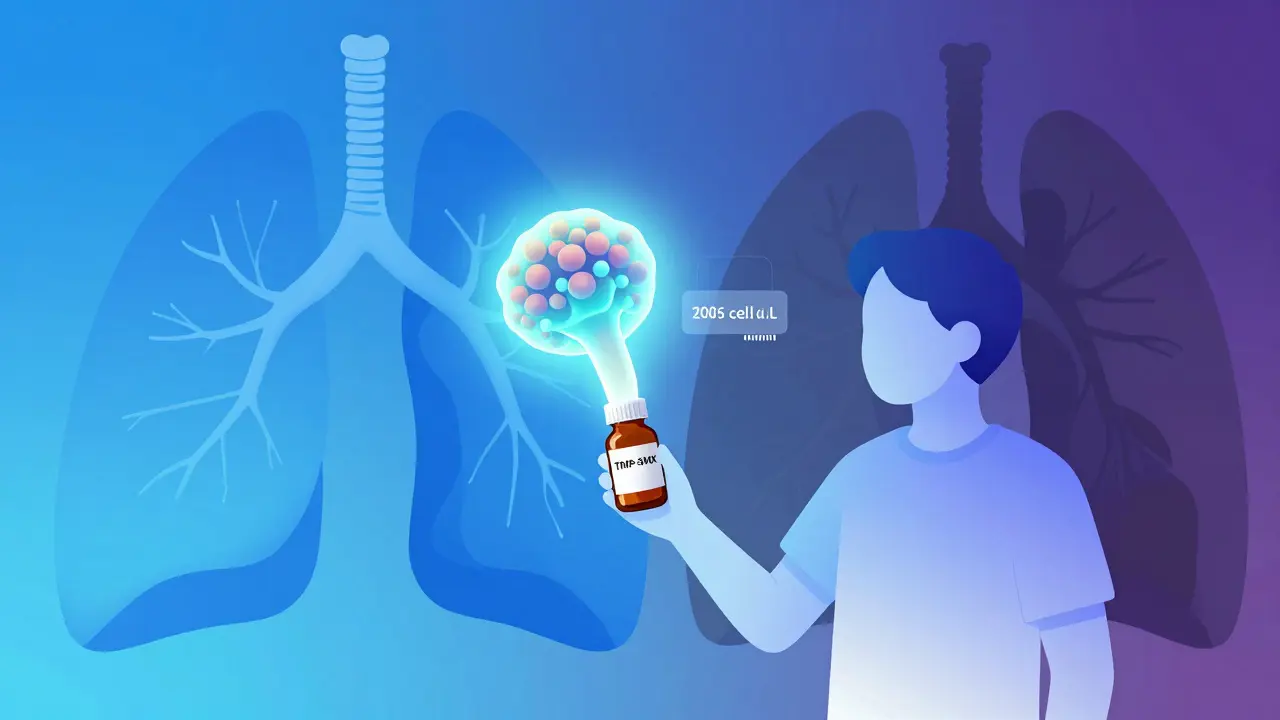
It’s not just about the dose. It’s about how much your body’s defenses are down. If your lymphocyte count is below 0.5 x 10⁹/L, or your CD4 count is under 200 cells/µL, your risk shoots up - even if you’re on a lower steroid dose. That’s why some hospitals now check blood counts before starting treatment. If your CD4 is low, you get prophylaxis. If it’s normal, you might not need it.
Some drugs are almost always a green light for prophylaxis:
- Cyclophosphamide - All patients get it, even after stopping the drug, for at least three months.
- Combination therapy - Steroids plus azathioprine, mycophenolate, or rituximab? That’s high risk. Even if each drug alone isn’t enough, together they can drop your defenses enough to let PCP take hold.
- Transplant recipients - Especially in the first year after surgery. These patients are on multiple drugs and often have low T-cell counts.
On the other hand, if you’re only on azathioprine or mycophenolate alone - no steroids - most guidelines say you’re low risk. But if you’ve had a recent infection, or your lymphocytes are low, that changes everything.
What’s the Best Way to Prevent It?
The gold standard is trimethoprim-sulfamethoxazole (TMP-SMX), sold as Bactrim or Septra. One double-strength tablet daily, seven days a week. It’s cheap - less than $200 a year - and it works. Studies show it cuts PCP risk by over 90%.
But here’s the catch: 20 to 30% of people can’t take it. Side effects include rash, nausea, liver issues, or low blood counts. If you’re allergic to sulfa drugs, you need alternatives:
- Dapsone - 100 mg daily. Watch out if you’re also on mycophenolate - both can suppress bone marrow.
- Atovaquone - 1500 mg daily in two doses. Expensive, but better tolerated.
- Aerosolized pentamidine - Inhaled once a month. Less effective than oral drugs, and not for pregnant women.
- Dapsone + pyrimethamine + leucovorin - Weekly combo for those who can’t tolerate daily pills.
Important note: Leucovorin is no longer needed with TMP-SMX unless you’re on high doses for treatment - not prevention. That’s a common mistake.
Why Are So Many People Not Getting Protected?
A 2018 study followed 316 patients with autoimmune diseases for over two years. Nearly 40% of those on high-risk drugs like cyclophosphamide got no prophylaxis at all. And guess what? None of them got PCP. Zero cases. That’s the big debate.
Some doctors say: if no one’s getting sick, why give everyone antibiotics? Side effects are real. Nausea, rashes, low white blood cells - they happen. One study found 2.2% of patients had a bad reaction per year. That’s 1 in 45 people every year. If PCP is super rare, maybe the risk of the drug outweighs the risk of the infection.
But here’s what that study didn’t tell you: those 316 patients were monitored closely. Their doctors knew the risks. They checked blood counts. They watched for symptoms. In a busy clinic with less follow-up, missing one case could be fatal. And PCP doesn’t just kill - it costs $25,000 to $65,000 to treat in the hospital. Prophylaxis? $150 a year.
Also, in real life, many patients don’t even know they’re at risk. A survey in rheumatology forums showed 40% of patients had never heard of PCP before their doctor mentioned it. That’s a communication failure.
What About Pregnancy and Long-Term Use?
If you’re pregnant and need prophylaxis, you still need protection - but avoid aerosolized pentamidine and atovaquone in the first trimester. TMP-SMX and dapsone are considered safe. Talk to your OB and specialist together. Don’t skip it just because you’re pregnant.
Long-term use of TMP-SMX? No evidence it causes antibiotic resistance in Pneumocystis. The fungus hasn’t evolved to fight it. But it can contribute to resistance in bacteria like E. coli or Staph - which is why some doctors hesitate. Still, the benefit outweighs the risk for high-risk patients. If you’re on it for years, get blood tests every few months to check your counts.
The Bottom Line: It’s Personal
There’s no one-size-fits-all answer. The old rule - “20 mg of prednisone for 4 weeks” - is a starting point, not a finish line. You need to look at the whole picture:
- What drugs are you on? (Steroids? Cyclophosphamide? Combination?)
- How long have you been on them?
- What’s your CD4 count? Lymphocyte count?
- Have you had recent infections or hospital stays?
- Can you tolerate TMP-SMX?
If you’re on high-dose steroids for more than a month - especially with another immunosuppressant - get tested. Ask for your CD4 and lymphocyte counts. If they’re low, prophylaxis is likely needed. If they’re normal and you’re on a low dose, talk to your doctor about whether you really need it.
And if you’re unsure? Ask for a referral to an infectious disease specialist. Rheumatologists, nephrologists, and transplant teams often have different standards. You deserve a clear, evidence-based plan - not guesswork.
What If You’ve Been on These Drugs for Years and Never Got Prophylaxis?
Don’t panic. If you’ve been on low-dose steroids (under 10 mg prednisone) for years, with normal blood counts and no other risk factors, your risk is extremely low. But if you’ve had a recent flare-up, started a new drug, or your lymphocyte count has dropped - get checked now. PCP doesn’t care how long you’ve been on meds. It only cares if your immune system is down.
Most people who’ve been on immunosuppressants for years without PCP are fine. But that doesn’t mean it won’t happen. Prevention is simple. Screening is easy. Don’t wait until you’re gasping for air to ask the question.
Do I need PCP prophylaxis if I’m on low-dose steroids?
Usually not - if you’re on less than 10 mg of prednisone daily and have no other risk factors like low CD4 or lymphocyte counts. But if you’re on steroids plus another immunosuppressant like azathioprine, even low-dose steroids can increase your risk. Always check your blood counts and talk to your doctor.
Can I stop prophylaxis if my immune system improves?
Yes - but only under medical supervision. If your CD4 count rises above 200 cells/µL and you’re off high-dose steroids, your doctor may consider stopping. For transplant patients, prophylaxis often continues for at least 6-12 months after reducing immunosuppression. Never stop on your own - PCP can come back fast.
Is trimethoprim-sulfamethoxazole safe for long-term use?
Yes, for most people. It’s been used for decades in HIV patients and transplant recipients. Side effects like rash or nausea are common early on but often improve. Blood tests every 2-3 months are recommended to check for low white cells or liver changes. There’s no evidence it causes Pneumocystis resistance.
What if I’m allergic to sulfa drugs?
You have options. Dapsone is the most common alternative, but avoid it if you’re also on mycophenolate. Atovaquone is well-tolerated but expensive. Aerosolized pentamidine is less effective and not recommended during pregnancy. Your doctor can help pick the best fit based on your health and drug history.
Why do some doctors not prescribe prophylaxis even when guidelines say to?
Because PCP is rare, and the drugs have side effects. Some doctors feel the risk of side effects outweighs the low chance of infection - especially if patients are closely monitored. But studies show many patients don’t get proper follow-up, and missing one case can be fatal. Guidelines exist because the cost of treating PCP is 100 times higher than preventing it.
Should I get tested for CD4 count if I’m on immunosuppressants?
If you’re on high-dose steroids, cyclophosphamide, or combination therapy - yes. CD4 count is one of the best predictors of PCP risk, even in non-HIV patients. Many rheumatology clinics now test it routinely. Ask your doctor to include it in your blood work if you’re on long-term immunosuppression.
What Comes Next?
Guidelines are changing. In 2025, the American Society of Transplantation is expected to release new rules. The IDSA is forming a working group to finally settle the debate on non-HIV patients. And research is showing that using CD4 counts as a trigger - not just steroid dose - could prevent unnecessary treatment in 35% of patients while still protecting those who need it.
For now, the safest move is simple: if you’re on high-dose steroids or cyclophosphamide, ask your doctor about PCP prophylaxis. Get your blood counts checked. Know your options. Don’t assume you’re safe just because you haven’t heard of this infection before. It’s silent. It’s deadly. But it’s preventable.




Iona Jane
January 15, 2026 AT 12:56