Parasite Immune Response Guide
Explore Parasite-Immune System Interactions
Select a parasite to see detailed information
Different parasites trigger different immune pathways. The Th1 pathway targets intracellular pathogens, while the Th2 pathway addresses large extracellular parasites.
When a parasitic infection is an invasion by organisms such as protozoa, worms, or arthropods that live at the expense of the host takes hold, the body’s immune system the network of cells, tissues, and organs that defends against pathogens jumps into gear. The battle isn’t a simple ‘good vs. bad’ fight; instead, parasites have evolved sophisticated tricks to dodge, suppress, or even hijack immune defenses. Understanding those tricks helps clinicians predict disease courses, design better vaccines, and manage long‑term health effects.
Why the Immune System Reacts Differently to Parasites
Unlike bacteria or viruses that often trigger rapid, high‑intensity inflammation, many parasites establish prolonged relationships with their hosts. This longevity forces the immune system to strike a balance between clearing the invader and limiting tissue damage caused by an overzealous response. Two major immune pathways dominate the conversation:
- Th1‑type immunity: Driven by interferon‑γ (IFN‑γ) and aimed at intracellular foes like Toxoplasma gondii a protozoan that lives inside cells and can cause encephalitis in immunocompromised people. This response activates macrophages and cytotoxic T cells.
- Th2‑type immunity: Characterized by interleukins‑4, ‑5, and ‑13, it promotes eosinophils, mast cells, and IgE production-perfect for tackling large extracellular parasites such as helminths.
Parasites can deliberately tip the scale toward the pathway that favors their survival. When they succeed, the host may experience chronic inflammation, allergic‑type symptoms, or immune suppression.
Major Parasite Classes and Their Immune Strategies
Below is a quick look at five common parasites, the class they belong to, and the typical immune pattern they provoke.
| Parasite | Class | Typical Immune Skew | Clinical Outcome |
|---|---|---|---|
| Plasmodium falciparum | Protozoa (malaria) | Th1‑dominant, high IFN‑γ | Severe anemia, cerebral malaria |
| Giardia lamblia | Protozoa (giardiasis) | Mixed Th1/Th2, secretory IgA | Acute watery diarrhea, malabsorption |
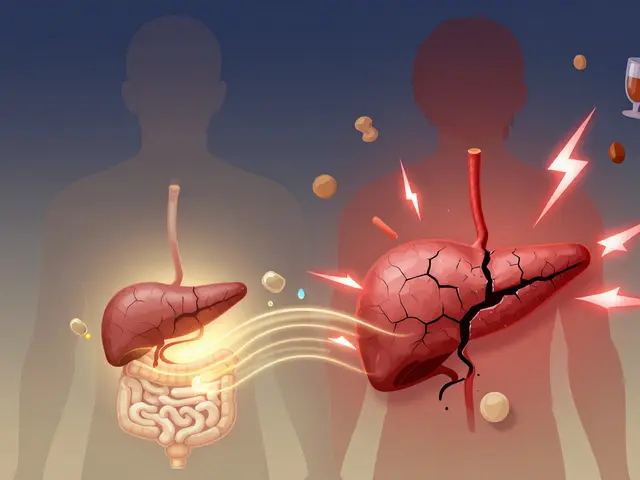
| Schistosoma mansoni | Helminth (trematode) | Strong Th2, eosinophilia | Liver fibrosis, bladder cancer risk |
| Ascaris lumbricoides | Helminth (nematode) | Th2 bias, high IgE | Intestinal obstruction, growth retardation |
| Toxoplasma gondii | Protozoa (intracellular) | Th1‑dominant, IFN‑γ | Congenital defects, encephalitis |
The table shows that even within a single class, individual species can drive subtly different responses. Clinicians often use these patterns to decide which laboratory markers to track-like eosinophil counts for helminths or serum IFN‑γ levels for intracellular protozoa.
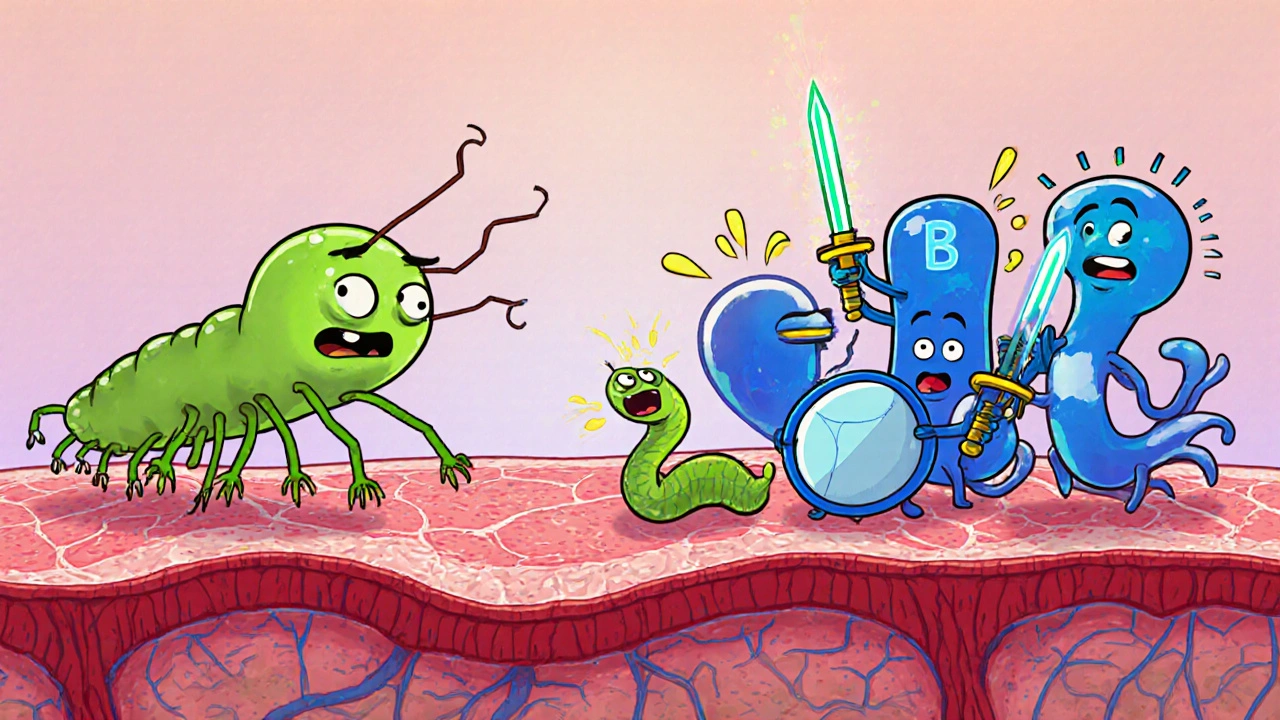
Helminths: Masters of Immune Modulation
Helminths (worms) have been living with humans for millennia. Their size and lifespan give them a unique evolutionary incentive to keep the host alive yet immunologically docile. They release excretory-secretory (ES) products that:
- Stimulate regulatory T cells (Tregs), which secrete IL‑10 and TGF‑β to dampen inflammation.
- Induce alternatively activated macrophages (AAMs) that promote tissue repair rather than killing.
- Shift antibody production toward IgE, which paradoxically limits severe tissue damage by “blocking” harmful Th1 cytokines.
These tricks can be a double‑edged sword. While they protect the host from severe pathology, they also create a permissive environment for co‑infections. For instance, patients with chronic schistosomiasis often show reduced vaccine responses to hepatitis B and influenza, likely because their immune system remains in a Th2‑biased, regulatory state.
Protozoa: Sneaky Intracellular Invaders
Protozoan parasites such as Plasmodium falciparum the deadliest malaria parasite, which invades red blood cells and liver hepatocytes or Toxoplasma gondii hide inside host cells to avoid antibody detection. Their main survival tactics include:
- Down‑regulating major histocompatibility complex (MHC) classI on infected cells, reducing CD8⁺ T‑cell recognition.
- Secreting effectors that interfere with the host’s NF‑κB signaling, thereby blunting pro‑inflammatory cytokine release.
- Manipulating host metabolism to create a nutrient‑rich niche, which indirectly suppresses immune activation.
Because these parasites rely on a strong Th1 response for clearance, patients with weakened IFN‑γ pathways (e.g., due to HIV or immunosuppressive drugs) often suffer severe or chronic disease.
Chronic Parasitic Infections and Immune Regulation
When an infection persists for months or years, the immune system settles into a new equilibrium. This can manifest as:
- Immune exhaustion: Persistent antigen exposure leads to up‑regulation of checkpoint molecules like PD‑1 on T cells, making them less responsive.
- Altered microbiome: Some helminths secrete antimicrobial peptides that shift gut bacterial populations, indirectly influencing systemic immunity.
- Increased susceptibility to autoimmunity: The regulatory environment can either protect against or exacerbate autoimmune disorders, depending on the parasite and host genetics.
Researchers are exploring “helminth therapy” for conditions like multiple sclerosis, where controlled infection might reset an overactive immune system. Early trials with Trichuris suis (the pig whipworm) showed modest reductions in disease activity, but the approach remains experimental.

Clinical Implications: Vaccines, Allergies, and Beyond
Understanding how parasites sculpt immunity has real‑world consequences:
- Vaccine efficacy: People living in endemic areas often need higher antigen doses or additional booster shots for vaccines against unrelated diseases, such as COVID‑19, because their immune system is constantly in a regulatory mode.
- Allergy prevalence: The “hygiene hypothesis” suggests that reduced helminth exposure in high‑income societies contributes to rising allergy rates. Some epidemiological studies report lower asthma incidence in children who grew up with helminth infections.
- Therapeutic targeting: Drugs that mimic helminth ES products (e.g., recombinant IL‑10 analogues) are being tested for inflammatory bowel disease and rheumatoid arthritis.
- Diagnostic clues: Elevated eosinophils, IgE spikes, or a specific cytokine signature can hint at an underlying parasitic cause when standard tests return negative.
Clinicians should therefore ask about travel history, water source, and pet contact when patients present with unexplained immune dysregulation.
Quick Checklist for Practitioners
- Ask about exposure risk (travel, sanitation, animal contact).
- Order stool ova‑and‑parasite exams for gastrointestinal symptoms.
- Check eosinophil count and serum IgE when a helminth is suspected.
- Consider measuring IFN‑γ or IL‑10 levels in chronic cases to gauge Th1/Th2 balance.
- Be aware that antiparasitic treatment may unmask underlying autoimmunity; monitor patients closely.
Frequently Asked Questions
Can a single parasite cause long‑term immune suppression?
Yes. Chronic helminth infections such as schistosomiasis can keep regulatory T cells activated for years, blunting responses to vaccines and other pathogens.
Do parasitic infections increase the risk of allergies?
In low‑resource settings, helminths tend to protect against allergies by promoting a Th2‑dominant, regulatory environment. Conversely, in high‑income countries, the lack of helminth exposure correlates with higher allergy rates.
Why do some patients with malaria have severe anemia while others do not?
The severity depends on host genetics, the balance between Th1 cytokines (which clear parasites) and inflammatory damage to red blood cells, and co‑infection with helminths that can modulate the immune response.
Can treating a helminth infection improve vaccine responses?
Studies show that deworming before influenza or hepatitis B vaccination can raise antibody titers, especially in children from endemic regions.
Is it safe to use helminth‑derived compounds as therapy?
Early‑phase trials suggest safety for low‑dose recombinant proteins, but large‑scale studies are still needed to confirm efficacy and rule out unintended immune suppression.




Macy-Lynn Lytsman Piernbaum
October 15, 2025 AT 21:44