You swallow a pill. It’s supposed to help your headache. But you feel worse. Not because the medicine doesn’t work - because you believe it doesn’t. This isn’t imagination. It’s science. And it’s happening every day with generic medications.
Identical Pills, Different Results
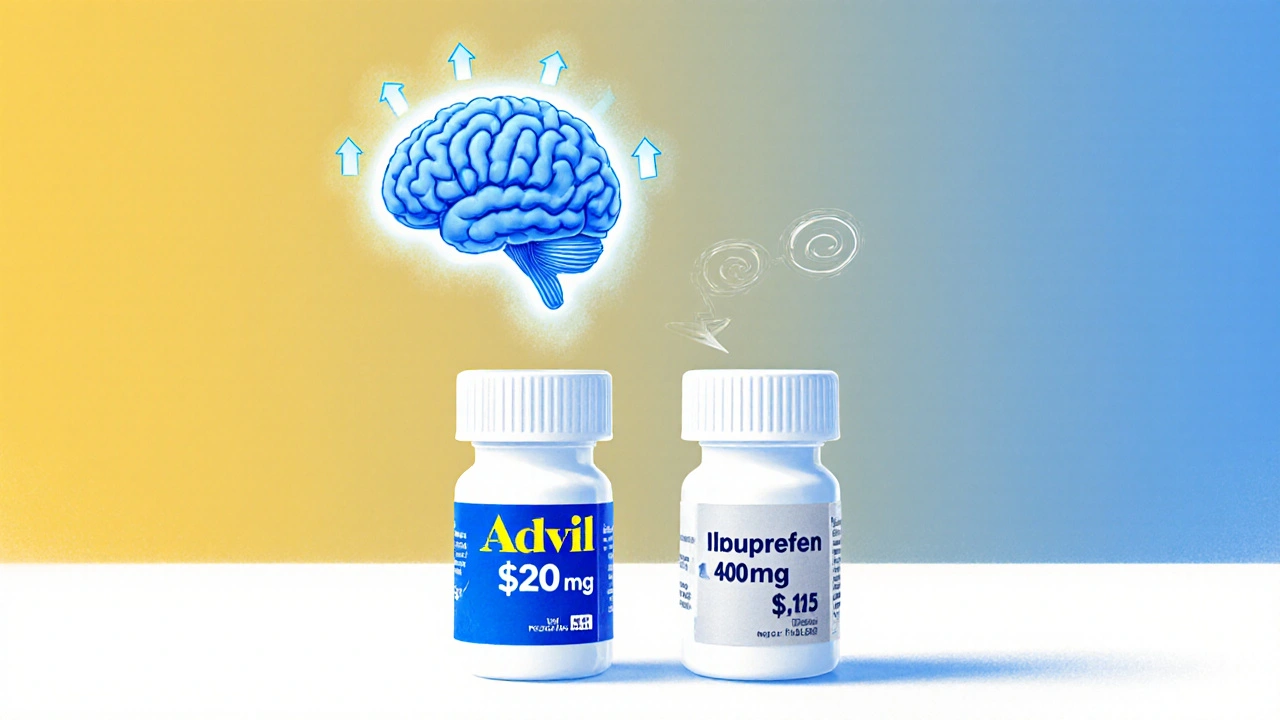
Two pills. Same active ingredient. Same dosage. Same manufacturer, sometimes even the same factory. One says "Ibuprofen 400mg" in plain white lettering. The other says "Advil" with bold blue packaging. One costs $0.15. The other costs $2.50.Now here’s the twist: both are sugar pills. No ibuprofen at all. But the one labeled "Advil" makes people feel better - significantly better - than the generic-labeled one. That’s not magic. That’s the placebo effect, twisted by perception.
A 2014 study at the University of Auckland gave 87 students fake painkillers. Half got the brand-labeled placebo. Half got the generic-labeled one. The brand-labeled group reported nearly twice the pain relief. The difference? Nothing in the pill. Everything in the mind.
Price Tells Your Brain What to Expect
Your brain doesn’t just react to chemicals. It reacts to signals. Price is one of the strongest signals.In a 2014 study at the University of Cincinnati, Parkinson’s patients were given fake injections. One group was told it cost $1,500 per dose. The other was told it cost $100. The $1,500 pill made them move better - 28% more improvement. Brain scans showed their dopamine levels spiked higher. The same dose. Same placebo. Different price. Different brain response.
That’s not about wealth. It’s about learned associations. We’ve been trained: expensive = better. This isn’t just true for cars or phones. It’s true for medicine. Even when we know better, our brains still listen.
Generic Labels Trigger the Nocebo Effect
The flip side of placebo is nocebo. That’s when negative expectations make you feel worse - even if nothing has changed.A 2014 meta-analysis of statin trials found people told they were taking a generic placebo reported more muscle pain than those told they were taking a brand-name placebo. Same pill. Same dose. But the label changed the experience. Generic = less trustworthy. Less effective. More side effects.
Real-world data backs this up. A 2017 JAMA study of 38,000 Medicare patients found those taking generics had 12-15% higher hospitalization rates than those on brand-name versions - even though the drugs were chemically identical. The only difference? Perception.
On Reddit, users report: "Switched to generic Nexium. My GERD came back." Or: "Generic Zoloft made me feel like I was drowning." Doctors check labs. They see normal levels. But the patient still feels worse. Why? Because their brain expected it to happen.
It’s Worse for Mental Health and Chronic Conditions
Some conditions rely more on the brain’s response than others. That’s why the placebo effect hits harder in depression, anxiety, migraines, and epilepsy.A 2013 review in Lancet Psychiatry found antidepressant trials with generic labeling had 11% lower response rates than brand-labeled ones - even when the pills were identical. Patients didn’t just feel worse. They were less likely to stick with treatment.
One study showed 18-24% higher discontinuation rates for psychiatric generics. Not because the drug failed. Because the patient believed it failed.
For migraine sufferers, brand-labeled placebos reduced pain by 41%. Generic-labeled placebos? Only 22%. That’s not a small gap. That’s the difference between going to work and staying in bed.
Generics Save Money - But Only If You Take Them
The math is clear: generics save $312 a year per patient on average. In 2023, 90% of U.S. prescriptions were filled as generics. That’s $265 billion in savings.But if patients stop taking them because they think they’re inferior, those savings vanish. And the cost shifts elsewhere - more ER visits, more missed work, more complications.
That’s why the real cost of the placebo effect isn’t just in pills. It’s in hospital bills. Lost productivity. Missed appointments. The system loses $1.2 billion a year because people choose brand names they don’t need.
Doctors Can Fix This - If They Know How
This isn’t a patient problem. It’s a communication problem.A 2018 study at the University of Chicago gave patients a 7-minute talk explaining bioequivalence: "This generic has the same active ingredient. It’s tested to work the same way. The only difference is the price." After that talk, generic acceptance jumped from 58% to 89%. Adherence stayed high six months later.
Another study trained doctors to use "positive generic messaging": "This version works exactly the same but saves you money." Patients on this approach had 85% adherence. Those given standard explanations? Only 63%.
It’s not about lying. It’s about reframing. Instead of saying, "We’re switching you to generic," say, "This is the same medicine, just cheaper. You’ll get the same results - and keep more money in your pocket."
Packaging and Tech Are Starting to Help
The system is slowly adapting. In 2023, a University of Wisconsin trial tested "premium" generic packaging - same pill, but design that looked more like brand-name products. Result? Nocebo complaints dropped by 37%.The FDA is also backing digital tools. A new app called "Generic Confidence" uses augmented reality to show patients how the active ingredient in a generic matches the brand. In testing, it boosted adherence by 29%.
Even blockchain is being tested. A 2024 NIH-funded study is exploring whether letting patients trace their generic pill back to its manufacturing source - with real-time quality data - can reduce distrust.
Who’s Most at Risk?
Not everyone feels this way the same way.Older adults are twice as likely to doubt generics. A 2023 AARP survey found 78% of patients over 65 worry about effectiveness. Younger people? Only 49%.
Low-income patients are hit hardest. They’re more likely to associate low cost with low quality. A 2023 JAMA Psychiatry study found they experience 2.3 times stronger nocebo effects. That’s not just about money. It’s about systemic distrust in healthcare.
And it’s worse for chronic conditions. You’re more likely to believe a generic blood pressure pill works than a generic antidepressant. Why? Because heart disease feels "real." Depression feels "in your head." And if it’s in your head, you think it’s easier to fake.
What You Can Do
If you’re on a generic:- Don’t assume it’s weaker. The science says it’s not.
- If you feel worse after switching, talk to your doctor - but don’t assume it’s the drug. Ask: "Could this be my expectations?"
- Ask for a quick explanation of bioequivalence. It takes less than five minutes.
- Keep track of symptoms. Write down how you feel before and after. Numbers beat feelings.
If you’re a doctor or caregiver:
- Don’t say, "This is just a generic." Say, "This is the exact same medicine, approved by the FDA to work the same way. It’s cheaper because it doesn’t have fancy ads."
- Use visuals. Show the FDA bioequivalence chart. Point to the identical active ingredient.
- Normalize the conversation. Make it part of every refill.
The Bigger Picture
We think medicine is about chemistry. It’s not. It’s about biology and belief.The placebo effect isn’t a flaw. It’s a feature of how humans work. And when we ignore it, we pay the price - in money, in health, in trust.
Generics aren’t second-rate. They’re the same medicine, priced right. But if we keep treating them like second-class options, our brains will make them feel that way.
The future of healthcare isn’t just better drugs. It’s better stories. Better explanations. Better trust.
Because sometimes, the most powerful medicine isn’t in the pill. It’s in the conversation before you take it.
Are generic drugs really the same as brand-name drugs?
Yes. By law, generic drugs must contain the same active ingredient, in the same strength, and work the same way in the body as the brand-name version. The FDA requires them to meet strict bioequivalence standards - meaning they deliver the same amount of medicine into your bloodstream at the same rate. The only differences are in inactive ingredients (like fillers), packaging, and price.
Why do some people feel worse on generic medications?
It’s often the nocebo effect - when expecting side effects or reduced effectiveness causes you to experience them. Studies show people told they’re taking a generic report more side effects than those taking the exact same pill labeled as brand-name. Your brain can trigger real physical symptoms based on what you believe, even if the drug hasn’t changed.
Can the placebo effect make generics work better?
Yes. If you believe a generic will work, your brain can enhance its effect. Studies show that when patients are told generics are identical to brand-name drugs, their outcomes improve. Positive framing - like "This works the same but saves you money" - boosts adherence and perceived effectiveness.
Do generics work for mental health conditions like depression?
They can - and do - for most people. But because mental health conditions are highly influenced by expectation and perception, the placebo effect plays a bigger role. Studies show slightly lower response rates in trials using generic labels, but real-world data from patients who are properly informed show nearly identical results. The key is communication: knowing the drug is equivalent helps your brain accept it.
Should I avoid generics because of the placebo effect?
No. Avoiding generics because of fear of reduced effectiveness means you’re paying more and risking worse outcomes. The placebo effect is real, but it’s fixable - through education, not avoidance. Most people experience no difference. For those who do, talking to their doctor often resolves it. Generics save billions in healthcare costs. They’re safe, effective, and widely used by millions.
What’s the best way to talk to my doctor about generics?
Ask: "Is this generic the same as the brand-name version?" and "How do we know it works the same?" Most doctors can show you FDA bioequivalence data. You can also say: "I’ve heard some people feel different on generics - is that common?" This opens the door to honest discussion. Don’t be afraid to ask for a short explanation - it takes minutes and can change your experience.



Andrew Forthmuller
November 11, 2025 AT 06:51