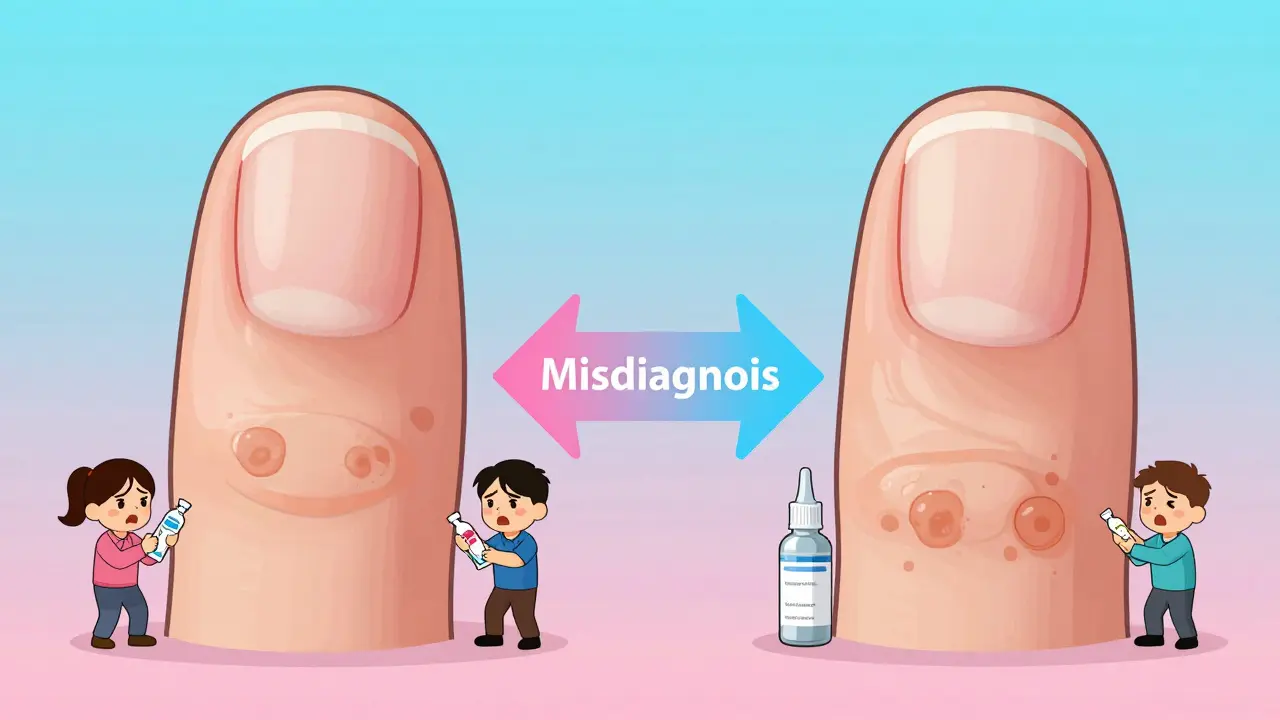
Most people assume that a thick, discolored nail is just a fungal infection. But what if it’s not? What if it’s something else entirely - something that won’t respond to antifungal creams, pills, or laser treatments? You’re not alone if you’ve spent months trying to fix your nails with over-the-counter solutions, only to see no improvement. That’s because fungal nail infection and nail psoriasis look nearly identical to the untrained eye - but they’re completely different conditions with totally different treatments.
What’s Really Going On With Your Nails?
Nail problems are more common than you think. Around 1 in 10 people will deal with a nail disorder at some point in their life. Two of the most frequent culprits are fungal infections and psoriatic changes. Both can make your nails yellow, crumbly, or detached from the skin underneath. But here’s the key difference: one is caused by a fungus, and the other is caused by your immune system attacking your own body. Fungal nail infections, or onychomycosis, happen when tiny organisms like Trichophyton rubrum invade your nail. They feed on keratin - the same protein that makes up your hair and nails. These fungi don’t just sit there. They spread slowly, starting at the tip or side of the nail, and over months, they turn the nail brown, black, or yellow. The nail gets thick, sometimes so thick you can’t cut it with regular clippers. You might even notice a foul smell - a classic sign that fungus is at work. Nail psoriasis, on the other hand, isn’t contagious. It’s part of psoriasis, an autoimmune disease. When your immune system goes haywire, it speeds up skin cell turnover. Instead of taking 28-30 days to renew, your skin cells regenerate every 3-4 days. These extra cells pile up under and around your nails, causing visible changes. You might see small pits - like pinpricks - on the surface. Or you might notice salmon-colored patches (translucent red-yellow spots) under the nail. Oil-drop lesions - small brownish spots that look like a drop of oil - are also common. Unlike fungal infections, psoriasis often hits multiple nails at once, and it usually shows up after you’ve already had skin psoriasis for years.How to Spot the Difference
If you’re trying to figure out what’s wrong, here are the red flags that point clearly to one condition or the other.- Nail pitting: If your nails have tiny dents or holes on the surface, it’s almost certainly psoriasis. This happens in about 70% of nail psoriasis cases and is extremely rare in fungal infections - only 2% of fungal cases show this.
- Foul odor: A bad smell coming from your nail? That’s a strong indicator of fungus. Psoriasis doesn’t cause odor. If your nails smell like something’s rotting, it’s likely not psoriasis.
- Location: Psoriasis tends to affect fingernails more than toenails. Fungal infections? They love toenails, especially the big toe. That’s because feet are warm, dark, and sweaty - perfect for fungi.
- Speed of change: Psoriasis can flare up suddenly. One day your nail looks fine; the next, it’s pitted and lifting. Fungal infections creep in slowly. You might not even notice for months until the discoloration spreads.
- Thickening: Both can thicken nails, but fungal infections usually cause more extreme thickening - often 3 to 5 millimeters. Psoriasis thickens nails too, but typically only to 2 to 3 millimeters.
There’s one more important clue: if you already have scaly, red patches on your elbows, knees, or scalp - you’re far more likely to have nail psoriasis. About 95% of people with nail psoriasis have had skin psoriasis first. If you’ve never had skin issues, a fungal infection is more likely.
Why Misdiagnosis Is So Common - and Costly
Doctors get this wrong a lot. Studies show that up to 40% of nail disorders are misdiagnosed. Why? Because they look too similar. A yellow, thickened nail is easy to label as fungus - especially if you’re not a dermatologist. A 2023 JAMA Dermatology study found that primary care doctors correctly identify these conditions only 52% of the time. Dermatologists? They get it right 85% of the time. The consequences? Wasted time, money, and frustration. People spend months using antifungal creams, soaking their feet, or even taking oral pills like terbinafine - all while their psoriasis gets worse. One Reddit user wrote: “I used antifungal treatments for 8 months. My nails got worse. Then I finally saw a dermatologist - it was psoriasis the whole time.” On the flip side, some people with fungal infections are told they have psoriasis and given steroid creams or injections. That doesn’t help - and can even make the fungus spread faster. A patient on FootHealthForum said: “They gave me steroid injections for psoriasis. My nail got more brittle, started crumbling. Turned out it was fungus.”
How Doctors Actually Diagnose These Conditions
You can’t tell the difference just by looking. That’s why doctors rely on simple, low-tech tests. The first step is a KOH (potassium hydroxide) test. A tiny clipping of your nail is scraped off and mixed with KOH solution. If fungus is present, it breaks down the nail cells and becomes visible under a microscope. This test is about 70-80% accurate and costs around $15-$25. If it’s negative but the doctor still suspects fungus, they’ll send a sample for fungal culture. That takes weeks but is 95% specific - meaning if it grows fungus, it’s definitely fungus. For psoriasis, there’s no single lab test. Diagnosis is based on appearance and medical history. Doctors use something called the NAPSI score - Nail Psoriasis Severity Index - which looks at four areas of the nail (the lunula, matrix, bed, and hyponychium) and assigns points for damage. A score of 0 means no damage. A score of 32 means severe involvement. In some cases, a biopsy or PAS staining (a special dye that highlights fungal elements) is used. These cost more - $75 to $125 - but are more accurate when the KOH test is unclear.What Works for Treatment
Treatment depends entirely on what you’re dealing with. Fungal infections: Oral antifungals like terbinafine are the gold standard. Most people see clearance after 12 weeks of daily use, confirmed by follow-up cultures. Topical treatments like efinaconazole (Jublia) work too, but they take 9 to 12 months - because toenails grow incredibly slowly, only about 0.1mm per day. You have to be patient. Keeping feet dry (humidity below 40%) and avoiding tight shoes helps prevent recurrence. Nail psoriasis: Antifungals won’t help. You need to treat the underlying immune issue. Topical steroids or corticosteroid injections under the nail can reduce inflammation and slow down nail changes. For moderate to severe cases, biologic drugs like secukinumab (Cosentyx) or ixekizumab are used. These target specific immune proteins and can improve nail appearance by 65% within 24 weeks. One 2022 CureTogether survey showed patients with nail psoriasis had dramatic improvement after starting biologics - something they never saw with antifungals.What You Can Do at Home
Regardless of the cause, good nail hygiene helps.- Keep nails trimmed short and clean.
- Avoid biting or picking at your nails - trauma can trigger psoriasis flares (this is called the Koebner phenomenon).
- Use moisturizers on your cuticles and nail folds. Dry skin around the nail can worsen separation.
- For fungal infections: wear breathable socks, change them daily, and use antifungal powder in shoes.
- For psoriasis: avoid harsh chemicals, wear gloves when washing dishes or cleaning.
Take monthly photos of your nails under consistent lighting. This helps you track changes over time and gives your doctor a clearer picture than a vague description.
What’s New in Diagnosis and Treatment
The field is changing fast. In 2023, Mayo Clinic tested reflectance confocal microscopy - a non-invasive imaging tool that can see nail structure in real time. It correctly identified psoriasis vs. fungus in 92% of cases. That’s better than most visual exams. In early 2024, the FDA approved Xepi (difloxacin) for superinfections in nail psoriasis - meaning if your psoriasis leads to a bacterial infection, you now have a targeted antibiotic. Future tools are even more exciting. Researchers at Mount Sinai are studying the nail microbiome. They found that psoriasis nails have more Staphylococcus bacteria and less Cutibacterium, while fungal nails show high levels of Trichophyton DNA. In a few years, a simple swab might tell you exactly what’s going on. AI-powered image analysis is also being tested. The Global Psoriasis Atlas predicts that by 2027, AI tools could cut misdiagnosis rates by 22% - meaning fewer people will waste months on the wrong treatment.When to See a Doctor
Don’t wait. If your nails have changed in the last few months - especially if you’re also dealing with skin symptoms like red, scaly patches - see a dermatologist. Don’t rely on online advice or pharmacy recommendations. The wrong treatment can make things worse. If you’ve tried antifungals for 3 months with no improvement, stop. It’s probably not fungus. Ask for a KOH test or referral to a specialist.Final Thoughts
Your nails are a window into your health. What looks like a simple cosmetic issue might be a sign of something deeper. Fungal infections and psoriatic changes are easy to mix up - but they need completely different care. Getting the right diagnosis isn’t just about fixing your nails. It’s about stopping the right problem before it spreads.Don’t guess. Get tested. And don’t let a misdiagnosis cost you months - or worse, your confidence.
Can nail psoriasis turn into a fungal infection?
Yes, it can. Nail psoriasis damages the nail structure, creating gaps and lifting where fungi can sneak in. About 4.6% to 30% of people with nail psoriasis develop a secondary fungal infection. That’s why doctors check for both - treating only one won’t fix the other.
Are fungal nail infections contagious?
Yes. Fungal nail infections can spread through shared towels, shoes, or public showers. Psoriasis is not contagious at all - you can’t catch it from someone else. That’s a key reason to get the right diagnosis before sharing personal items.
How long does it take to treat nail psoriasis?
Topical treatments like corticosteroid injections can show improvement in 8 to 12 weeks. Biologics like secukinumab take longer - around 24 weeks for full results. Because nails grow slowly, you may still see damage for months after treatment starts. Patience is essential.
Can I treat both conditions at the same time?
If you have both - which happens in up to 30% of psoriasis patients - yes. A dermatologist can prescribe antifungals to clear the fungus and biologics or steroids to manage the psoriasis. Treating only one will leave the other untreated, so both need to be addressed together.
Why do some nail treatments fail even when the diagnosis is right?
Nails grow slowly - especially toenails. Even if the treatment is working, you won’t see results until the damaged part grows out completely. That can take 6 to 12 months. Also, if you stop treatment early because you don’t see immediate change, the infection or inflammation can come back. Stick to the full course.




Alexandra Enns
January 24, 2026 AT 11:47