Most people don’t realize how much they rely on hearing until it starts to fade. You might notice you’re asking people to repeat themselves, turning up the TV too loud, or struggling to follow conversations in noisy rooms. These aren’t just signs of aging-they could be early warnings of hearing loss. The only way to know for sure is through audiometry testing, a simple, non-invasive procedure that measures exactly how well you hear different sounds.
What Is Audiometry Testing?
Audiometry testing is the gold standard for checking your hearing. It’s not a quick screen-it’s a detailed assessment that maps your hearing sensitivity across different pitches, from low rumbles to high-pitched tones. The results are plotted on a graph called an audiogram, which shows exactly which frequencies you hear well and which ones you miss.
The test uses pure tones-clean, single-frequency sounds-played through headphones or a small device behind your ear. You’ll hear beeps, buzzes, and chirps at varying volumes. Each time you hear one, you signal by raising your hand or pressing a button. The goal isn’t to hear every single sound, but to find the quietest level you can detect about half the time. That’s called your threshold.
These thresholds are measured in decibels hearing level (dB HL). Zero dB HL doesn’t mean silence-it’s the average softest sound a healthy young adult can hear. Normal hearing is defined as 25 dB HL or better across all tested frequencies. If your threshold is 40 dB at 2000 Hz, that means you need sounds to be 40 decibels louder than what most people with perfect hearing can detect. That’s a moderate hearing loss, and it’s enough to make speech unclear, especially consonants like s, t, and k.
How Audiometry Works: Air vs. Bone Conduction
There are two main ways sound reaches your inner ear: through the air, and through your bones. Audiometry tests both.
Air conduction is the most common part of the test. Sound travels through your outer ear, vibrates your eardrum, and moves through tiny bones in your middle ear before reaching the cochlea. This tests your entire hearing pathway.
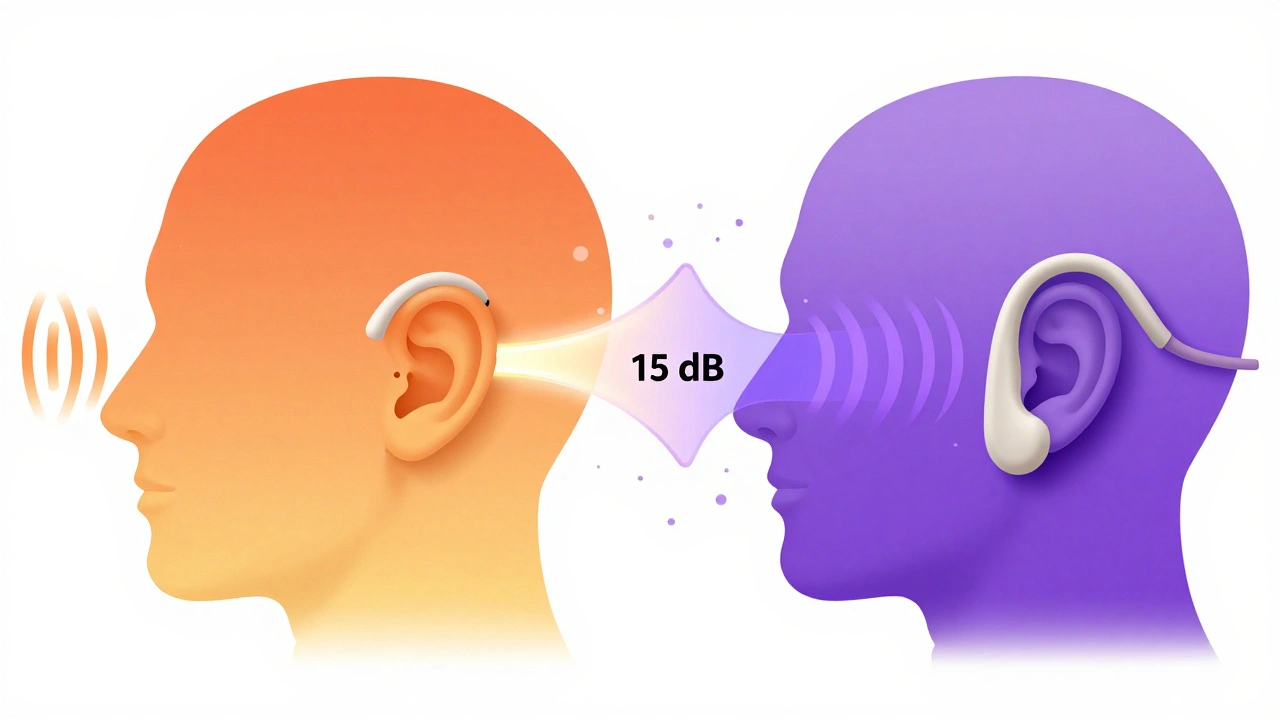
Bone conduction skips the outer and middle ear entirely. A small vibrator is placed behind your ear, on the mastoid bone. It sends vibrations directly to the cochlea. If your bone conduction thresholds are normal but your air conduction thresholds are worse, that means something is blocking sound in your outer or middle ear-like earwax, fluid from an infection, or a perforated eardrum. This is called conductive hearing loss.
If both air and bone conduction are equally poor, the problem is in the inner ear or auditory nerve. That’s sensorineural hearing loss, the most common type, often caused by aging, noise exposure, or genetics. The difference between air and bone thresholds is called the air-bone gap. A gap of 15 dB or more at any frequency confirms conductive loss.
The Hughson-Westlake Method: Precision in Action
Not all audiometry is the same. The standard technique used in clinics today is the modified Hughson-Westlake method, developed in the 1940s and still the most reliable way to find your true hearing threshold.
Here’s how it works: The audiologist starts with a tone you can easily hear-say, 40 dB at 1000 Hz. Then they lower the volume by 10 dB. If you don’t hear it, they go back up 5 dB. They keep adjusting in small steps until they find the exact point where you hear the tone about half the time. This method is slow, but it’s accurate. Screening tests that just check if you hear a tone at one volume can miss early hearing loss.
The test usually follows a set order: 1000 Hz, 2000 Hz, 4000 Hz, 8000 Hz, then 500 Hz, 250 Hz. Each ear is tested separately. The whole process takes 10 to 15 minutes per ear. It’s not painful, but it can feel tedious. That’s why audiologists often use visual cues or games for children, and make sure adults are well-rested and focused.
Speech Testing: More Than Just Beeps
Hearing a beep doesn’t tell you if you can understand speech. That’s why every full audiometry test includes speech testing.
Speech Reception Threshold (SRT) measures the quietest level at which you can repeat 50% of two-syllable words correctly. For most people, this number should be within 10 dB of the average of their pure-tone thresholds at 500, 1000, and 2000 Hz. If your SRT is much worse than your pure-tone results, it could point to a problem with the auditory nerve or brain processing.
Word Recognition Score (WRS) tells you how well you understand speech when it’s loud enough to hear. You’ll repeat lists of single-syllable words at a volume 25-40 dB above your threshold. A score of 90-100% is normal. If you’re at 60% or lower, even with hearing aids, you’ll still struggle to follow conversations. This is especially common in people with noise damage or age-related hearing loss.
Some people have normal audiograms but still say, “I can hear people, but I can’t understand them.” That’s usually a sign of poor word recognition. Audiometry catches this-something a basic hearing screening never will.
Tympanometry and ABR: The Supporting Tests
Audiometry doesn’t stop at tone and speech tests. A full evaluation often includes two more tools.
Tympanometry checks your middle ear. A small probe seals your ear canal and changes the air pressure while playing a tone. It measures how well your eardrum moves. A flat result (called a Type B tympanogram) often means fluid is trapped behind the eardrum-common in kids with ear infections or adults with Eustachian tube dysfunction. It takes just a few seconds and is completely painless.
Auditory Brainstem Response (ABR) is used when the patient can’t respond reliably-like babies, young children, or people with cognitive delays. Electrodes on the scalp record how the brainstem reacts to clicks or tones. It doesn’t require any cooperation from the patient. ABR is the gold standard for newborn hearing screening. In the U.S., 95% of newborns get screened before leaving the hospital, thanks to CDC guidelines.
What Your Audiogram Tells You
Your audiogram is a map of your hearing. The horizontal axis shows frequency-from low (250 Hz) on the left to high (8000 Hz) on the right. The vertical axis shows volume in dB HL, with softer sounds at the top.
Circle symbols mean air conduction in your right ear. X’s mean left ear. Brackets mean right bone conduction. Less-than signs mean left bone conduction.
Here’s what patterns mean:
- Flat loss: Equal hearing loss across all frequencies-common with aging.
- High-frequency loss: Trouble with high pitches like birdsong or “s” sounds-classic noise damage or presbycusis.
- Notch at 4000 Hz: A dip right at 4000 Hz is a telltale sign of noise-induced hearing loss.
- Conductive dip: A gap between air and bone thresholds, especially at low frequencies, suggests middle ear issues.
Audiologists use these patterns to diagnose the cause. For example, a 4000 Hz notch in a 50-year-old construction worker points to noise exposure. A flat loss in a 70-year-old with no noise history points to age-related decline.
Who Needs Audiometry Testing?
You don’t need to wait until you’re struggling to get tested. Here’s who should consider it:
- Anyone over 50-regular checkups every 2-3 years are recommended.
- People exposed to loud noise at work or leisure-construction, music, hunting, motorcycling.
- Those with a family history of hearing loss.
- Anyone taking ototoxic medications-like certain antibiotics or chemotherapy drugs.
- People with diabetes, heart disease, or high blood pressure-these conditions can affect inner ear blood flow.
- Parents of children who don’t respond to their name, talk late, or turn up the TV.
The CDC recommends that all newborns get screened before leaving the hospital. If they fail, diagnostic audiometry should be done by three months old. Early intervention can prevent language delays.

Common Misconceptions and Pitfalls
Many people think hearing loss is just about volume. It’s not. It’s about clarity. You might hear someone talking, but miss the difference between “cat” and “hat.” That’s why speech testing is just as important as tone testing.
Another myth: “I’ll know if I’m losing my hearing.” You won’t. Hearing loss creeps in slowly. Your brain adapts. You start avoiding noisy restaurants, not because you hate crowds, but because your ears can’t keep up.
Some patients skip follow-up because the test was “fine.” But audiometry is a baseline. If your hearing is normal now, you should get retested every few years. If it’s not, you need to track changes over time to know if hearing aids or other treatments are working.
And don’t assume retail hearing aids are enough. Many stores offer quick screenings, but they don’t test speech recognition, bone conduction, or middle ear function. Without that data, you might get a hearing aid that amplifies everything-but doesn’t improve understanding.
What Happens After the Test?
A good audiologist doesn’t just hand you a paper with squiggly lines. They explain what the numbers mean in plain language. They show you your audiogram and point out where you’re missing sounds. They tell you if hearing aids could help-and if so, what kind.
If you have mild to moderate hearing loss, hearing aids are often the next step. For conductive loss, medical treatment like earwax removal or surgery might be needed. For severe loss, cochlear implants may be an option.
But the real value of audiometry isn’t just the device you get. It’s knowing exactly what’s happening. One patient told me, “I thought I was just bad at listening. Turns out, my ears were failing me. Now I know why.” That clarity changes everything.
Future of Audiometry: AI and Telehealth
Audiometry is evolving. New software uses artificial intelligence to analyze audiograms and flag patterns-like a 4000 Hz notch or air-bone gap-with 87% accuracy. Some devices now let you test your hearing at home using smartphone apps and calibrated headphones.
But home tests have limits. They can’t measure bone conduction or speech recognition reliably. They’re good for tracking known loss, not diagnosing new problems. For that, you still need a licensed audiologist with a calibrated booth and proper protocols.
Tele-audiology is growing, especially in rural areas where audiologists are scarce. But the gold standard-clinical audiometry with masking, bone conduction, and speech testing-is still best done in person. Technology helps, but it doesn’t replace expertise.
Final Thoughts: Hearing Is a Skill-And It Can Be Measured
Hearing isn’t just about volume. It’s about timing, clarity, and brain processing. Audiometry doesn’t just tell you if you can hear-it tells you how well you understand. And that’s the difference between hearing someone and truly listening to them.
If you’ve been wondering why conversations feel harder than they used to, or if you’ve been told you speak too loudly, don’t ignore it. Get tested. It takes less than 20 minutes. The results could change how you connect with the people around you-for the better.






Anna Roh
December 10, 2025 AT 17:23