Medication Side Effect Frequency Calculator
See Side Effect Frequencies
The FDA's new Patient Medication Information (PMI) rule requires clear side effect data. Enter a common medication name to see real-world frequency data.
The FDA's new PMI requires side effect data to be presented clearly - not just 'may occur' but with actual frequencies like "43% of patients report headaches" as mentioned in the article.
The U.S. Food and Drug Administration (FDA) is proposing a major shift in how patients receive information about their prescription drugs. Right now, most people get a small paper insert or a pharmacy label with basic instructions. But under the new Patient Medication Information (PMI) rule, every outpatient prescription - from antibiotics to blood pressure meds - will come with a single-page, standardized document designed to be clear, consistent, and easy to understand.
Why the FDA Is Changing the Rules
Right now, only about 150 prescription drugs in the U.S. are required to come with a Medication Guide. That’s less than 10% of all prescriptions. The rest? Patients get whatever the pharmacy decides to print - often a label focused on dosage, refill info, or insurance codes, not safety. This inconsistency has real consequences. According to the Institute of Medicine, medication errors cause around 1.3 million injuries and 7,000 deaths each year in the U.S. Many of these errors happen because patients don’t fully understand how to take their drugs, what side effects to watch for, or how to store them safely. The FDA’s new PMI rule aims to fix that. It’s not just about adding more paper. It’s about making sure every patient, no matter where they fill their prescription, gets the same clear, accurate, and essential information. The goal is simple: reduce preventable harm by giving people the facts they need to use their meds safely.What the New PMI Will Look Like
The PMI isn’t just a rewrite of old Medication Guides. It’s a complete redesign based on patient testing and plain language research. Here’s what it must include:- A bold header that says: “Use exactly as prescribed”
- Clear directions on how to take the drug - including when, how often, and whether to take it with food
- How to store the medication - like keeping it away from heat or moisture
- How to safely dispose of unused pills - no more flushing them down the toilet
- Key safety warnings - such as avoiding alcohol or not driving while on the drug
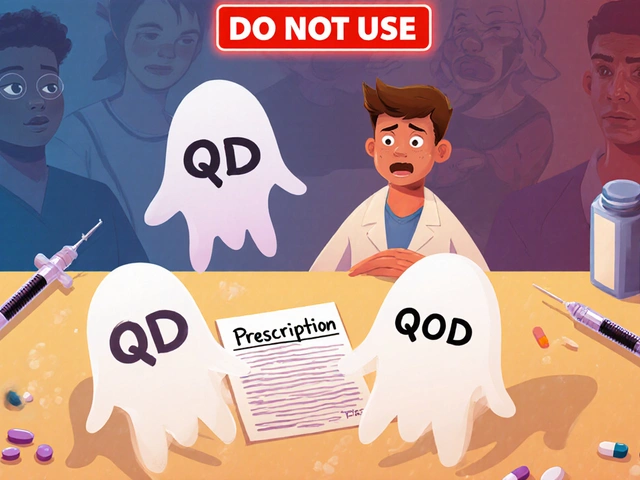
- A list of common side effects - but not vague terms like “may occur.” The FDA is leaning toward more specific language based on testing
Electronic PMI Is Coming Too
You won’t always get a paper copy. The FDA now allows electronic delivery - through pharmacy apps, patient portals, or email - as long as it’s accessible. That means the digital version must meet Section 508 accessibility standards: readable by screen readers, resizable text, no flashing graphics, and available in multiple languages if needed. This change reflects how people actually get information today. But the FDA is clear: paper must still be offered. Not everyone has a smartphone, reliable internet, or the ability to navigate digital systems. The rule is designed to be inclusive.
What’s Missing? The Criticisms
Not everyone thinks the PMI goes far enough. Researchers at the University of Pittsburgh tested their own version - called “Decision Critical PMI” - and found patients wanted more. For example, instead of saying “headache is a common side effect,” they argued for: “43% of patients report headaches.” That specificity helps people decide if the side effect is likely to affect them or just a rare chance. They also pointed out that the FDA’s version doesn’t mention the drug’s benefits or how well it works. If you’re taking a medication for depression, you might want to know: “This drug helps 60% of people feel better within 6 weeks.” Right now, that info is left to the doctor’s conversation - but what if the patient didn’t fully understand that talk? The PMI might be the only written resource they have. The FDA acknowledges these concerns. In public meetings, they said they’re open to future updates. But for now, they’re prioritizing safety and clarity over comprehensive drug education. Their focus is on preventing immediate harm - not replacing doctor visits.Who Has to Do What?
This isn’t just a paperwork change. It’s a system-wide overhaul.- Pharmaceutical companies will have to create, submit, and update PMIs for every outpatient prescription they make - potentially tens of thousands of documents. They’ll have 24 to 36 months to comply, depending on company size.
- Pharmacies will need to add PMI distribution to their workflow. That’s an extra 30-60 seconds per prescription during the first year. Staff will need 2-4 hours of training, plus annual refreshers.
- Health providers will need to make sure their prescribing practices align with the PMI content. If a doctor tells a patient to take a drug twice a day, but the PMI says once, that’s a problem.

What This Means for Patients
For you, the patient, this change could mean fewer surprises and more confidence. Imagine picking up your new diabetes medication and seeing the same clear instructions whether you go to CVS, Walgreens, or a local pharmacy. No more guessing if the pill you’re holding is the right one. No more wondering if the nausea you feel is normal or dangerous. The PMI doesn’t replace the doctor’s advice - but it reinforces it. Studies show patients who get clear written instructions are 30% more likely to take their meds correctly. That means fewer hospital visits, fewer side effects, and better control of chronic conditions. Patient advocacy groups like the National Patient Safety Foundation say this change could prevent up to 30% of outpatient medication errors - about 230,000 incidents a year. That’s not just numbers. That’s people avoiding falls, trips to the ER, and even death.What’s Next?
The proposal was published in May 2023. The public comment period closed in November 2023, with over 1,200 responses from patients, doctors, pharmacists, and drug companies. The FDA is now reviewing those comments. Industry experts predict the final rule will be published in early 2024, with full implementation starting in 2025. The FDA has hinted that future updates might include benefit data and more detailed side effect rates - especially if research like the University of Pittsburgh’s shows patients understand better with that info. This isn’t the end of the story. It’s the beginning of a new standard.International Watch
The European Medicines Agency (EMA) is watching closely. They’re considering a similar standardized patient information system for 2025. If the U.S. succeeds, it could become a global model. Other countries have tried - but none have gone this far in making medication information uniform, mandatory, and patient-first. This change isn’t just about labels. It’s about trust. When patients can read and understand their meds, they feel more in control. And when they feel in control, they’re more likely to stick with their treatment - and stay healthy.Will every prescription drug have a PMI?
Yes. The proposed rule requires PMI for all outpatient prescription drugs, including those taken by mouth, injected, or given as a transfusion. This covers everything from antibiotics to insulin to blood pressure pills. The only exceptions are drugs used only in hospitals or emergency settings.
Can I still get a paper copy if I prefer it?
Yes. The FDA requires pharmacies to offer a printed PMI even if you choose to receive it electronically. This ensures accessibility for people without smartphones, internet access, or vision impairments.
Will the PMI tell me how well the drug works?
Not in the first version. The current proposal focuses on safety, usage, and side effects. It does not include information on how effective the drug is or how it works in the body. Some researchers argue this is a gap, and the FDA has said it may consider adding benefit data in future updates based on patient feedback.
When will the PMI be required?
The final rule is expected in early 2024. Large manufacturers must comply within 24 months of publication, and smaller ones have 36 months. Most pharmacies and patients should start seeing the new PMIs in 2025.
How is the PMI different from the old Medication Guide?
Medication Guides are only required for about 150 high-risk drugs, and their format varies widely. The PMI will be mandatory for all outpatient prescriptions and follow one strict, tested format - one page, plain language, standardized layout - ensuring consistency no matter where you get your prescription.






Paul Dixon
December 10, 2025 AT 14:48