Every year, more than 1.5 million people in the U.S. are harmed by medications-not because they’re taking the wrong drug, but because of preventable mistakes. That’s more than the population of Cleveland or Pittsburgh. And it’s not just happening in hospitals. It’s happening in your kitchen, at the pharmacy counter, and even when you’re following your doctor’s instructions exactly.
Medication Errors Are More Common Than You Think
You might assume that if you take your pills as directed, you’re safe. But the truth is, medication errors happen at every step: when a doctor writes the prescription, when a pharmacist fills it, when a nurse gives it in the hospital, and when you take it at home. The World Health Organization says about 1 in 20 patients worldwide experiences harm from medication use. That’s 5%. Multiply that by the number of people taking prescriptions globally, and you’re looking at tens of millions of avoidable injuries each year.
In the U.S., that translates to 1.3 million people harmed annually. And it’s not just side effects. These are errors-wrong dose, wrong drug, wrong timing, or a dangerous interaction you weren’t warned about. At least 7,000 people die each year in U.S. hospitals alone because of these mistakes. That’s more than traffic accidents in some years.
Which Medications Are Most Dangerous?
Not all drugs carry the same risk. Some are far more likely to cause harm if used incorrectly. According to WHO’s 2024 analysis, antibiotics are behind about 20% of all medication-related harm. Why? Because they’re overprescribed, often for viral infections they can’t treat. When people take them unnecessarily, it leads to resistance-and when they’re taken wrong, they can cause severe allergic reactions or deadly gut infections like C. diff.
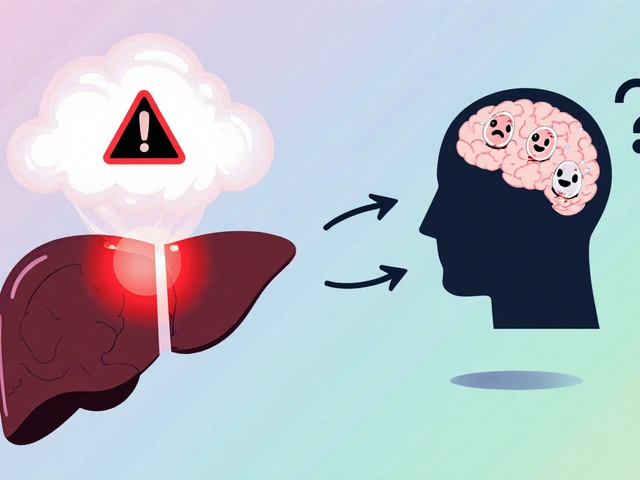
Next up: antipsychotics (19%), central nervous system drugs like sedatives and anti-anxiety meds (16%), and cardiovascular drugs like blood thinners and beta-blockers (15%). These are high-risk because they have narrow safety margins. A little too much warfarin can cause internal bleeding. A little too much insulin can send you into a coma. A little too much benzodiazepine can slow your breathing to a stop.
And then there’s the growing threat of counterfeit drugs. In the U.S., nearly 32% of all fake drug seizures happen here. Between 2019 and 2021, more than 55% of overdose deaths involving oxycodone were from fake pills laced with fentanyl. In 2023, the DEA seized over 80 million fake fentanyl tablets. These pills look identical to real prescriptions-but they’re deadly.
What Happens at Home? The Hidden Risks
Hospitals get a lot of attention, but most medication errors happen at home. A 2025 analysis by SingleCare found that between 2% and 33% of patients make mistakes with their medications when taking them themselves. That’s a huge range because it depends on age, education, and complexity of the regimen.
Common mistakes:
- Taking two doses instead of one because you forgot you already took it
- Stopping antibiotics early because you “feel better”
- Crushing pills that shouldn’t be crushed
- Mixing alcohol with painkillers or sleep aids
- Not knowing what a new medication is for
One Reddit thread analyzing over 1,200 patient posts found that 68% of concerns were about confusion over dosage instructions. Another 22% were about side effects that weren’t clearly explained by their doctor. If you don’t know why you’re taking a drug or what to watch for, you’re flying blind.

Who’s Most at Risk?
Older adults are the most vulnerable. People over 65 take an average of 14 prescriptions per year. That’s a lot of pills, a lot of timing, a lot of interactions. In Australia, efforts to cut down on antipsychotic use in seniors led to an 11% drop in inappropriate prescriptions between 2016 and 2021. That’s because those drugs can cause falls, confusion, and even sudden death in elderly patients.
Children are also at risk. A child given an adult dose of acetaminophen can suffer liver failure. A teenager misusing stimulants like Adderall for focus can develop heart problems or addiction. And people with mental health conditions often take multiple drugs that interact badly-especially if they’re seeing multiple doctors who don’t talk to each other.
What’s Being Done-and What’s Not Working
There are efforts to fix this. The World Health Organization launched its Medication Without Harm campaign in 2017, aiming to cut severe medication errors by 50% by 2026. So far, 134 countries have created national plans. Australia has made real progress: a 37% drop in opioid deaths since 2018 thanks to real-time prescription tracking. The U.S. is rolling out new CMS safety measures for 2025, tracking things like statin use in diabetics and antipsychotic use in dementia patients.
But big problems remain. Infusion pumps-devices that deliver IV drugs-had over 200,000 reported events between January 2023 and August 2024, including 204 deaths. Why? Because they’re complicated, poorly programmed, and often used without proper training. And counterfeit drugs are getting smarter. Fake pills now come with QR codes that mimic real packaging. You can’t tell the difference unless you scan them-and most people don’t.
As Dr. Donald Berwick, a leading patient safety expert, put it: “Most medication errors are system failures, not individual failures.” Blaming a nurse or a patient misses the point. The system is broken. Too many handoffs. Too little communication. Too few checks.

What You Can Do to Protect Yourself
You can’t fix the system alone-but you can protect yourself. Here’s how:
- Keep a living medication list. Write down every drug you take-including vitamins, supplements, and over-the-counter pills. Update it every time your doctor changes something. Bring it to every appointment.
- Use one pharmacy. A single pharmacy can check for dangerous interactions between all your meds. If you use multiple pharmacies, they can’t see what the others are dispensing.
- Ask the “5 Ws” for every new prescription: What is this for? Why am I taking it? What are the side effects? What happens if I miss a dose? What should I avoid while taking it?
- Check the pill. If your pill looks different than last time, ask the pharmacist. Fake pills are everywhere. Real pills have consistent color, shape, and markings.
- Don’t skip the pharmacist. Pharmacists are medication experts. They can explain how to take it, warn about interactions, and tell you if the dose seems off.
- Use pill organizers with alarms. Especially if you take 5+ meds a day. Set reminders on your phone too.
- Never share prescriptions. A pill that helps your friend’s anxiety could kill you.
The Australian Commission on Safety and Quality in Health Care recommends the “5 Moments for Medication Safety”: when you start a new drug, when you add one, when you move between care settings (like hospital to home), when you’re on high-risk meds, and when you review all your meds every 6 months.
The Future: Technology Can Help-If Used Right
AI-powered tools are being developed to catch errors before they happen. One study predicts that smart medication reconciliation systems could reduce mistakes by up to 30% by 2027. These systems automatically compare your current meds with what’s being prescribed and flag risks.
But tech alone won’t fix this. The real solution is better communication, more patient education, and a culture that doesn’t punish mistakes but learns from them. If your doctor doesn’t take the time to explain your meds, ask again. If your pharmacist seems rushed, insist on a consultation. Your life depends on it.
Medication safety isn’t just a hospital problem. It’s a personal responsibility. And the best defense? Knowledge. Questions. And never assuming anything.
How common are medication errors in the U.S.?
More than 1.5 million Americans are harmed by medication errors each year, with around 1.3 million of those cases being preventable. These errors cause at least 7,000 deaths annually in hospitals alone, and contribute to over 1.5 million emergency room visits. The majority of these errors happen outside hospitals-in homes, pharmacies, and clinics.
What are the most dangerous types of medications?
Antibiotics cause about 20% of medication-related harm, often due to misuse or allergic reactions. Antipsychotics (19%), central nervous system drugs like sedatives (16%), and cardiovascular drugs like blood thinners (15%) are also high-risk. These medications have narrow safety margins-small mistakes can lead to serious injury or death. Counterfeit drugs laced with fentanyl are now among the deadliest, especially for younger adults.
Why are older adults more at risk?
Older adults typically take 14 or more prescriptions per year, increasing the chance of drug interactions, dosing errors, and side effects. Many are prescribed antipsychotics or sedatives for behavioral issues, which can cause confusion, falls, and sudden death. In Australia, reducing inappropriate antipsychotic use in seniors led to an 11% drop in prescriptions between 2016 and 2021, showing that targeted interventions work.
Can fake drugs really kill you?
Yes. Counterfeit pills, especially those sold online or through social media, are often laced with fentanyl-a synthetic opioid 50 to 100 times stronger than morphine. In 2023, the DEA seized over 80 million fake fentanyl tablets. Between 2019 and 2021, more than half of all oxycodone-related overdose deaths involved fake pills. These drugs look identical to real prescriptions but can kill in minutes.
What should I do if my pill looks different?
Never take it. Call your pharmacy immediately. Pill appearance-including color, shape, size, and imprint code-is carefully controlled. If it changes without explanation, it could be counterfeit, a different drug, or a wrong dose. Pharmacists are trained to verify these details. Ask them to confirm the medication matches your prescription.
How can I prevent medication errors at home?
Keep an updated list of all your medications-including supplements-and bring it to every appointment. Use one pharmacy for all your prescriptions. Ask your doctor and pharmacist the five key questions: What is this for? Why am I taking it? What are the side effects? What if I miss a dose? What should I avoid? Use a pill organizer with alarms. Never crush pills unless instructed. And never take someone else’s medicine.





Mark Alan
January 27, 2026 AT 13:56