How and Where to Buy Norvasc Online: Safe Options in 2025
July 9 2025Retail Pharmacy Mistakes: Common Errors and How to Avoid Them
When you pick up your prescription at the retail pharmacy, a local pharmacy where medications are dispensed to patients under the supervision of licensed pharmacists. Also known as community pharmacy, it's meant to be a safe last step in your care—but it's also where things can go wrong. A misplaced decimal, a confusing abbreviation, or an unchecked drug interaction can turn a simple refill into a medical emergency. These aren’t rare glitches. Studies show that over 1.5 million preventable medication errors happen in U.S. pharmacies each year, and many start at the counter.
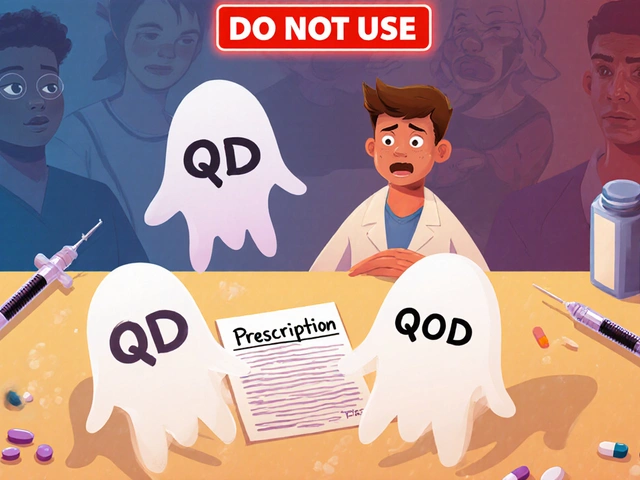
One of the biggest problems is prescription errors, mistakes in how medications are written, filled, or labeled. Think abbreviations like "QD" (once daily) mistaken for "QID" (four times daily), or "MS" confused as morphine instead of magnesium sulfate. The FDA’s "Do Not Use" list exists for a reason—these shortcuts still show up on handwritten and even digital scripts. Then there’s generic substitution, when a pharmacist swaps a brand-name drug for a cheaper generic version. For most drugs, this is fine. But for narrow therapeutic index (NTI) drugs like warfarin, phenytoin, or levothyroxine, even tiny differences in absorption can cause dangerous spikes or drops in blood levels. Patients don’t always know they’ve been switched, and doctors don’t always monitor closely enough.
And let’s not forget drug interactions, when two or more medications react in harmful ways. A patient on blood thinners might pick up an OTC allergy pill that increases bleeding risk. Someone with kidney disease might take Tums for heartburn, not realizing it can cause aluminum toxicity. Pharmacists are trained to catch these, but they’re stretched thin. A busy counter, a rushed refill, or a poorly organized system can mean red flags get missed. Even labeling errors—like mixing up similar-looking bottles—can lead to the wrong drug going to the wrong person.
These aren’t just pharmacy problems. They’re patient problems too. You’re not powerless. Always ask: "Is this the same as last time?" Check the pill color, shape, and name. Compare the label to your doctor’s instructions. If something feels off, speak up. Bring a list of everything you take—prescription, OTC, supplements—to every visit. And if you’re switching generics, especially for heart, seizure, or thyroid meds, ask your doctor to monitor your levels.
What follows are real cases and hard truths pulled from studies and patient reports. You’ll find guides on dangerous abbreviations, why some generics make people feel worse, how antihistamines can increase fall risk in seniors, and what to do when you miss a blood thinner dose. This isn’t theory. It’s what’s happening in pharmacies right now—and how you can protect yourself before it’s too late.
 22 Nov
22 Nov
Medication Errors in Hospitals vs. Retail Pharmacies: What Really Happens Behind the Counter
Medication errors happen in both hospitals and retail pharmacies, but the causes, frequency, and consequences differ greatly. Hospitals have more errors but better safety nets. Pharmacies have fewer errors - but patients are often the last line of defense.
Read More...