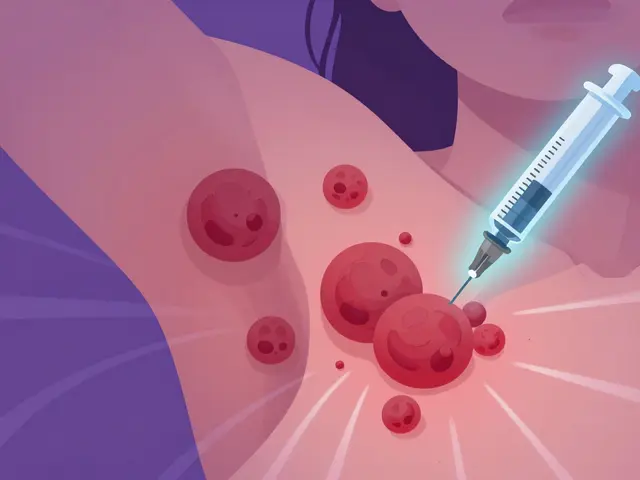
Hidradenitis Suppurativa: Painful Nodules and Biologic Therapy Explained
December 20 2025Brand-Name Medication: What It Is, Why It Matters, and What You Should Know
When you pick up a prescription, you might see the brand-name medication, a drug sold under a proprietary name by the original manufacturer, often with a patent-protected formula and marketing. Also known as originator drug, it’s the version your doctor first prescribes — but it’s not always the only option. Many people assume brand-name means better, but the truth is more complicated. The FDA requires generics to match brand-name drugs in active ingredients, strength, and how they work in the body. So why do some patients feel worse on generics? It’s not chemistry — it’s placebo effect, the psychological impact of believing a drug is more effective because of its brand, packaging, or cost. Studies show that people report stronger side effects or reduced effectiveness with generics — even when the pills are chemically identical. This isn’t weakness. It’s how the brain processes medicine.
Then there’s the NTI drugs, narrow therapeutic index medications where tiny changes in dosage can cause serious harm or treatment failure. These include warfarin, phenytoin, and levothyroxine. For these, switching from brand to generic isn’t just a cost decision — it’s a safety one. Research shows that even small differences in how generics are absorbed can cause dangerous spikes or drops in blood levels. Hospitals and specialists often stick with brand-name versions for NTI drugs, not because they’re superior, but because the margin for error is razor-thin. And when you’re managing a condition like epilepsy or heart rhythm, that margin matters.
It’s not just about science. medication safety, the system of practices designed to prevent errors in prescribing, dispensing, and taking drugs plays a huge role too. A pill’s color, size, or even the shape of the logo can affect whether someone remembers to take it — especially in older adults or people with cognitive challenges. Cultural beliefs matter: some patients refuse generics because they look "cheap" or because their family always took the brand. Language on the label, religious concerns about ingredients, or distrust in manufacturers all influence whether a drug is actually taken. That’s why a pill that works perfectly in a lab might fail in real life.
Brand-name medication isn’t inherently better. But it’s not just a marketing trick either. Sometimes, it’s the safest, most reliable option — especially for critical conditions. Other times, the generic works just as well, and saving money means you can afford to take it consistently. The real question isn’t brand vs. generic. It’s: What works for you, safely, and sustainably? Below, you’ll find real stories, studies, and practical advice on how to navigate this choice — whether you’re managing heart disease, depression, or chronic pain. No fluff. Just what you need to know.
 25 Nov
25 Nov
How to Appeal Insurance Denials for Brand-Name Medications
Learn how to successfully appeal insurance denials for brand-name medications with step-by-step guidance, real success rates, and critical tips from doctors and legal experts. Know your rights and how to win.
Read More...