HE Probiotic Efficacy Calculator
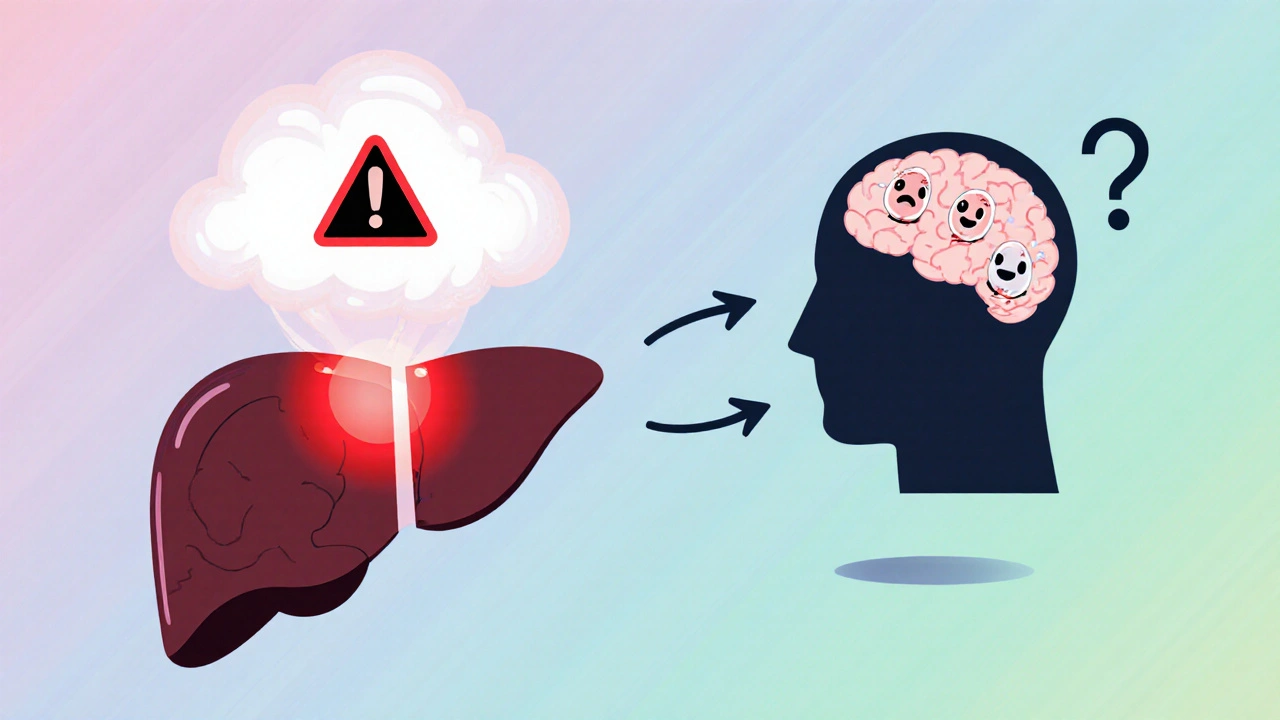
When the liver can’t clear toxins, the brain suffers - that’s the reality of Hepatic Encephalopathy is a neuropsychiatric complication of advanced liver disease, marked by confusion, mood swings, and even coma. Probiotics are live microorganisms that, when taken in adequate amounts, confer health benefits by reshaping the gut ecosystem. In recent years, clinicians have asked whether probiotics for hepatic encephalopathy can blunt toxic buildup and improve cognition. This guide walks through the science, the evidence, and practical steps for anyone facing this challenging condition.
What Triggers Hepatic Encephalopathy?
HE arises when a failing liver can’t detoxify ammonia and other gut‑derived metabolites. The key steps are:
- Protein breakdown in the gut produces ammonia.
- Normally, the liver converts ammonia to urea, which is excreted.
- In cirrhosis, portal hypertension forces blood to bypass the liver (portosystemic shunting), leaving ammonia in circulation.
- Ammonia crosses the blood‑brain barrier, altering neurotransmission and causing the hallmark mental changes.
Other culprits include inflammatory cytokines, manganese accumulation, and alterations in the gut microbiota - an ecosystem now recognized as a major player in HE.
Standard Pharmacologic Approaches
Two drugs dominate current guidelines:
- Lactulose - a non‑absorbable sugar that acidifies the colon, trapping ammonia as ammonium for excretion.
- Rifaximin - a broad‑spectrum, gut‑restricted antibiotic that reduces ammonia‑producing bacteria.
Both improve survival and quality of life, but they come with drawbacks. Lactulose can cause bloating, diarrhea, and adherence issues. Rifaximin, while better tolerated, adds a significant cost burden and may promote antibiotic resistance over the long term.
How Probiotics Might Help
Probiotics target the gut microbiome directly. Their proposed mechanisms include:
- Competing with ammonia‑producing organisms such as Enterobacteriaceae.
- Producing short‑chain fatty acids that lower colonic pH, similar to lactulose’s effect.
- Enhancing mucosal barrier integrity, reducing bacterial translocation and inflammation.
- Modulating immune responses that amplify neurotoxicity.
Key genera studied in HE are Lactobacillus and Bifidobacterium, often delivered as multi‑strain blends.
Clinical Evidence - What Do the Trials Say?
Since 2018, several randomized controlled trials (RCTs) have examined probiotic regimens either alone or in combination with lactulose. Highlights:
- Indian 2020 trial (n=80): A daily capsule containing Lactobacillus rhamnosus GG and Bifidobacterium longum reduced mean ammonia levels by 22 % after 12 weeks versus placebo (p<0.01). Cognitive scores (Stroop test) improved by 1.8 points.
- European multicenter study 2022 (n=214): Adding a 3‑strain probiotic to standard lactulose shortened time to HE reversal from 6.2 days to 4.1 days (hazard ratio 1.45). No serious adverse events were recorded.
- Meta‑analysis 2024 (15 RCTs, 1,350 patients): Probiotics lowered serum ammonia by an average of 15 µmol/L and reduced HE recurrence risk by 30 % (RR 0.70). Heterogeneity stemmed mainly from strain differences and treatment duration.
While promising, the data are not uniform. Studies using single strains often show modest effects, whereas multi‑strain preparations tend to perform better.
Choosing the Right Probiotic Regimen
When evaluating a probiotic for HE, consider four attributes:
| Attribute | Probiotics (multi‑strain) | Lactulose | Rifaximin |
|---|---|---|---|
| Primary mechanism | Modulate gut flora & lower ammonia production | Acidify colon, trap ammonia | Suppress ammonia‑producing bacteria |
| Typical efficacy (ammonia reduction) | 15‑25 % (clinically modest) | 30‑40 % | 35‑45 % |
| Side‑effect profile | Generally mild - bloating, flatulence | Diarrhea, cramping | Rare GI upset; potential resistance |
| Cost (per month, US$) | 30‑60 | 15‑25 | 350‑550 |
| Regulatory status | Dietary supplement (Food‑grade) | Prescription medication | Prescription antibiotic |
For most patients, probiotics are best used as an adjunct, not a replacement, to lactulose or rifaximin. The decision hinges on disease severity, tolerance, and financial considerations.
Practical Tips for Patients and Caregivers
- Start low, go slow. Begin with one capsule daily and monitor for bloating.
- Pick a clinically studied blend. Look for products that list specific strains (e.g., L. rhamnosus GG, B. longum BB536) and CFU counts ≥10⁹.
- Stick to the schedule. Probiotic benefits accrue over weeks; aim for at least 8 weeks before judging effectiveness.
- Combine with diet. Moderate protein intake, high‑fiber foods, and low‑sodium meals support gut health.
- Watch for interactions. If you’re on rifaximin, maintain a wash‑out period of 24 hours before starting a probiotic to avoid competitive colonization.
- Regular labs. Have your clinician check ammonia levels and liver function every 2-3 months while on any new supplement.

Potential Pitfalls and When to Stop
Probiotics are safe for most adults, but be cautious if you have:
- Severe immunosuppression - rare cases of bacteremia have been reported.
- Short‑bowel syndrome - altered transit may change strain survival.
- Allergy to dairy or soy, which are common carriers in capsule fillers.
If you notice worsening confusion, persistent diarrhea, or new abdominal pain, pause the probiotic and contact your hepatology team promptly.
Future Directions
Research is moving beyond generic blends toward personalized microbiome therapy. Ongoing trials (e.g., 2025 NEJM study) are testing next‑generation probiotics engineered to consume ammonia directly. Fecal microbiota transplantation (FMT) also shows early promise, but safety concerns keep it in the experimental realm.
Quick Checklist: Integrating Probiotics into HE Management
- Confirm diagnosis of hepatic encephalopathy (clinical grade 2 or higher).
- Ensure baseline lactulose or rifaximin regimen is optimized.
- Select a multi‑strain probiotic with ≥10⁹ CFU per dose.
- Start with one capsule daily; increase to two after 2 weeks if tolerated.
- Track symptoms weekly (confusion score, bowel habits).
- Re‑measure serum ammonia at 8‑week mark.
- Adjust or discontinue based on clinical response and side‑effects.
Can probiotics replace lactulose in treating hepatic encephalopathy?
Current evidence suggests probiotics work best as an add‑on to lactulose, not as a standalone replacement. They can lower ammonia modestly and improve cognition, but lactulose remains the first‑line therapy for most patients.
What probiotic strains have the strongest data for HE?
Multi‑strain blends that include Lactobacillus rhamnosus GG and Bifidobacterium longum (or their equivalents) have the most robust trial data. Single‑strain products show inconsistent results.
Are there safety concerns for patients with advanced cirrhosis?
Probiotics are generally safe, but patients with severe immunosuppression or recent gastrointestinal bleeding should use them under close medical supervision. Rare cases of bloodstream infection have been reported.
How long should a probiotic be taken for HE?
Most studies evaluate an 8‑ to 12‑week course. If you experience benefit and tolerate it well, clinicians often suggest continuation as a maintenance strategy, reassessing every 6 months.
Do probiotics interact with rifaximin?
There is no strong drug‑drug interaction, but both target gut microbes. Some clinicians stagger dosing (e.g., rifaximin in the morning, probiotic in the evening) to avoid competitive colonization.





Matthew Hall
October 20, 2025 AT 17:10