Sirolimus Timing Calculator
This calculator helps determine the optimal time to start sirolimus after transplant surgery based on patient-specific risk factors and surgical type. Using evidence-based guidelines from the article, it provides personalized recommendations for timing sirolimus administration.
Recommended Sirolimus Start Time
Key considerations:
- For major abdominal surgery: Typically 7-14 days post-op (longer for high-risk patients)
- For minor procedures: May start as early as day 5 with careful monitoring
- Higher BMI (>30) increases risk by nearly 30% per 5-point increase
- Smoking cessation for 4 weeks before surgery cuts risk in half
When a patient gets a kidney transplant, the goal isn’t just to keep the new organ alive-it’s to keep them alive and healthy for years after. That’s where sirolimus comes in. It’s an immunosuppressant that helps prevent organ rejection without damaging the kidneys, unlike older drugs like tacrolimus. But there’s a catch: sirolimus can slow down wound healing. And if you give it too soon after surgery, you might end up with a wound that won’t close, an infection, or even a dehiscence-where the incision splits open.
How Sirolimus Slows Down Healing
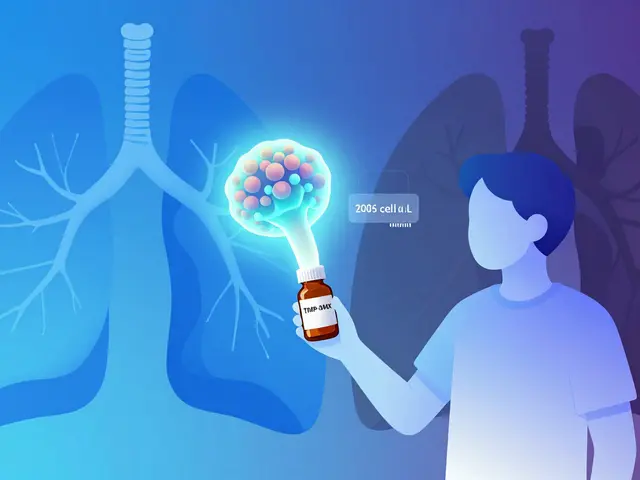
Sirolimus, also known as rapamycin, works by blocking the mTOR pathway. That’s a key cellular switch that tells cells to grow, divide, and repair. In transplant patients, that’s useful-it stops the immune system from attacking the new organ. But in a surgical wound, that same blockage hurts healing. Studies in rats show that when sirolimus is given at doses used in humans, wound strength drops by up to 40%. Collagen, the protein that acts like scaffolding for new tissue, doesn’t build up properly. Blood vessels don’t form as they should because sirolimus cuts down on VEGF, the signal that tells the body to grow new capillaries. Without those tiny blood vessels, the wound doesn’t get enough oxygen or nutrients to heal. It’s not just about blood vessels. Fibroblasts-cells that make connective tissue-and smooth muscle cells also stop multiplying. The result? A wound that looks okay on the surface but is weak underneath. It’s like building a house with weak beams. You might not notice until it’s too late.When Do Surgeons Wait?
Most transplant centers don’t start sirolimus right after surgery. The standard practice is to wait 7 to 14 days. That’s not arbitrary. It’s based on what happens in the body during those first two weeks. The first 72 hours are critical for inflammation and early tissue repair. By day 7, collagen starts to form in earnest. By day 14, the wound has reached about 70% of its final strength. Give sirolimus before then, and you’re interrupting the most important phase of healing. A 2009 review in Frontiers Partnerships recommended avoiding sirolimus during the first week after transplant. That advice still holds for most patients-especially those having major abdominal surgery. But it’s not a hard rule anymore. The old fear that sirolimus always causes bad wounds is fading.Who’s at Highest Risk?
Not everyone who takes sirolimus gets wound problems. The risk depends on the person. Obesity is the biggest red flag. A higher BMI means more tension on the wound, less blood flow to fatty tissue, and more inflammation. One study found that for every 5-point increase in BMI, the odds of a wound complication went up by nearly 30%. That’s why surgeons often delay sirolimus even longer for patients with a BMI over 30. Other risk factors are modifiable-and that’s good news. Diabetes, smoking, malnutrition, and alcohol use all make healing worse. A patient who quits smoking four weeks before surgery cuts their risk of poor healing in half. Correcting low protein levels before surgery helps too. These aren’t just lifestyle tips-they’re medical interventions. Age is a factor, but not the main one. Older patients heal slower, but it’s the combination of age plus diabetes plus obesity that creates real danger. That’s why doctors now look at the whole picture, not just the drug.
What About Other Drugs?
Sirolimus doesn’t work alone. It’s usually part of a cocktail with steroids, mycophenolate, or antithymocyte globulin (ATG). And guess what? Most of those also slow healing. Steroids, for example, suppress inflammation-the same process that kicks off healing. Mycophenolate stops immune cells from multiplying. ATG wipes out T-cells. So when you add sirolimus on top, you’re stacking multiple healing blockers. That’s why some centers use a “step-down” approach: start with calcineurin inhibitors (like tacrolimus) right after surgery, then switch to sirolimus once the wound is stable. Others use sirolimus from day one but keep the dose low-under 4 ng/mL-and monitor blood levels closely.Is Sirolimus Still Worth It?
Yes. For the right patient, it’s one of the best tools available. About 15-20% of kidney transplant patients take sirolimus. Why? Because it doesn’t hurt the kidneys. Tacrolimus and cyclosporine, the other main options, can cause long-term kidney damage. For someone who’s already lost one kidney, that’s a big deal. Sirolimus also lowers cancer risk. Transplant patients have a 2-4 times higher chance of developing skin cancer, lymphoma, and other tumors. Sirolimus has real anti-cancer properties. One study showed a 50% drop in new skin cancers among patients switched to sirolimus. The key is matching the drug to the patient. A 55-year-old with a history of squamous cell carcinoma and normal kidney function? Sirolimus makes sense. A 35-year-old with obesity, diabetes, and a recent abdominal transplant? Maybe not yet.
What’s Changing Now?
The old advice-“don’t use sirolimus until 14 days post-op”-is being rewritten. A 2008 Mayo Clinic study looked at 26 transplant patients who got sirolimus after dermatologic surgery. The wound dehiscence rate was 7.7%. That sounds high. But the control group had zero dehiscence. The difference wasn’t statistically significant. Why? Because these were small skin procedures, not big abdominal cuts. That’s the breakthrough: context matters. The risk isn’t the same for a hand surgery as it is for a liver transplant. A 2022 review in Wiley called earlier concerns about sirolimus “old myths.” The new reality? With careful dosing, monitoring, and patient selection, wound complications can be minimized. Now, centers are testing low-dose sirolimus (2-4 ng/mL) starting as early as day 5. They’re using VEGF levels as a biomarker. They’re checking protein levels before surgery. They’re delaying sirolimus only for high-risk patients-not everyone.What Should You Do?
If you’re a patient:- Ask if your transplant team has a protocol for sirolimus timing.
- If you smoke, quit at least 4 weeks before surgery.
- Get your blood sugar and protein levels checked before the operation.
- Ask about your BMI and whether it affects your risk.
- Don’t assume sirolimus is off-limits-ask why it’s being delayed or avoided.
- Don’t use a one-size-fits-all delay. Tailor timing to the surgery type and patient risk.
- Monitor sirolimus trough levels-keep them below 6 ng/mL in the first 30 days.
- Use nutritional support and smoking cessation as part of pre-op planning.
- Consider switching from calcineurin inhibitors to sirolimus after 7-10 days if the wound is healing well.
Final Thought
Sirolimus isn’t the villain in wound healing. It’s a tool. And like any tool, its danger comes from misuse-not the tool itself. The goal isn’t to avoid sirolimus. It’s to use it smarter. With better data, better monitoring, and better patient prep, we can get the benefits-better kidney function, lower cancer risk-without the wounds that won’t heal.It’s not about waiting longer. It’s about waiting wisely.






Shae Chapman
December 31, 2025 AT 10:32