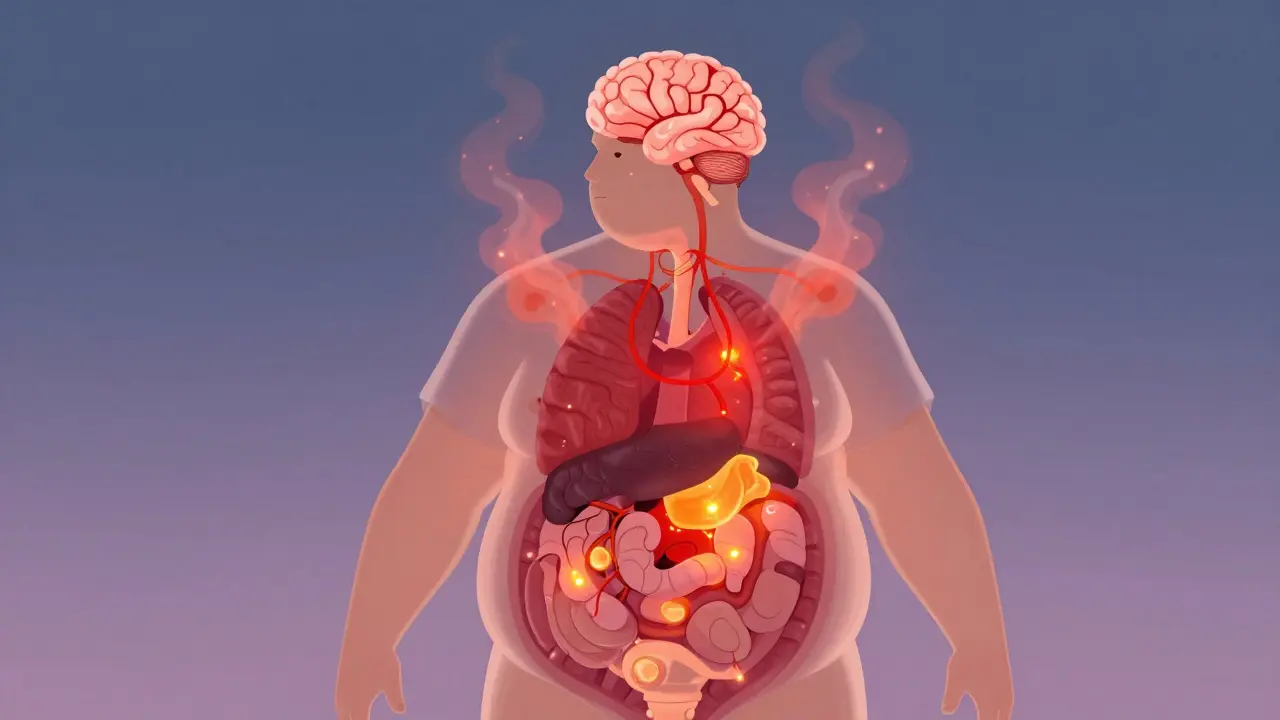
Obesity isn’t just about being overweight. It’s a chronic disease - one that rewires your brain, disrupts your hormones, and slowly damages your organs. For decades, it was treated like a failure of willpower. But science has moved past that. Today, we know obesity is driven by biology, not laziness. It’s not something you can simply ‘eat less and move more’ your way out of. And if you’ve tried diets before and ended up heavier than before, you’re not broken. Your body is responding exactly as it’s designed to.
Why Obesity Is Classified as a Chronic Disease
In 2013, the American Medical Association officially labeled obesity a disease. That wasn’t just a change in wording - it was a shift in how doctors are supposed to treat it. The World Health Organization defines obesity as a BMI of 30 or higher, but that number alone doesn’t tell the whole story. Two people with the same BMI can have wildly different metabolic health. One might have normal blood pressure, insulin levels, and liver function. The other might already have early signs of type 2 diabetes and fatty liver disease.
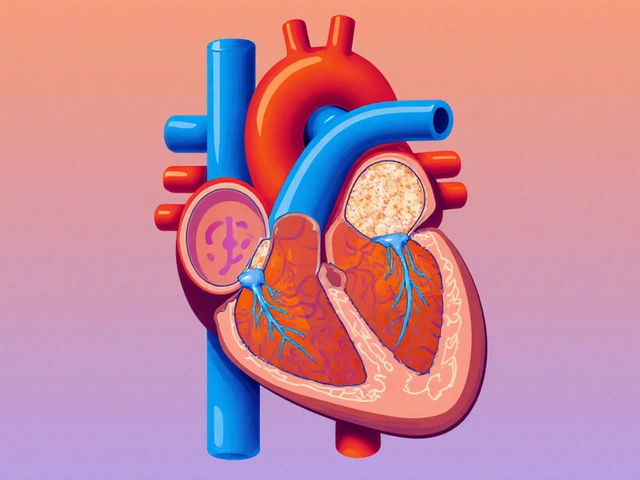
The real problem isn’t just fat on the outside - it’s fat that’s acting like a toxic organ inside. Fat tissue in people with obesity releases inflammatory chemicals, disrupts insulin signaling, and alters hunger hormones. Studies show obese individuals have 2 to 3 times higher levels of C-reactive protein, a marker of systemic inflammation. That’s why obesity is linked to 13 types of cancer, heart disease, stroke, and severe arthritis. It’s not a side effect - it’s the cause.
And it’s progressive. Once you reach a certain point, your body fights to stay there. The more weight you gain, the more your metabolism slows down. Your brain gets better at craving high-calorie foods. Sleep gets worse. Stress hormones rise. It becomes harder to move, which means you burn even fewer calories. This isn’t a cycle you can break with willpower alone. It’s a biological trap.
The Hidden Biology Behind Weight Gain
Genetics play a huge role. Twin studies show 40 to 70% of obesity risk comes from your genes. Over 250 genetic variants have been linked to body weight. Some people naturally have higher levels of ghrelin - the hunger hormone - or lower levels of leptin - the fullness signal. Others have mutations in the MC4R gene, which affects how the brain regulates appetite. These aren’t rare. MC4R mutations are found in 2 to 5% of people with severe obesity.
Then there’s the gut. Research now shows your microbiome - the trillions of bacteria in your digestive system - can influence how you store fat and how hungry you feel. People with obesity often have less of a specific bacteria called Faecalibacterium prausnitzii, which helps reduce inflammation. When that’s missing, your body stays in a low-grade inflammatory state, making weight loss harder.
And sleep? It’s not optional. People with obesity sleep, on average, 30 to 45 minutes less per night than those without. Less sleep means more ghrelin, less leptin, and stronger cravings for sugar and carbs. It’s not that people with obesity are lazy - they’re exhausted. And exhaustion makes healthy choices feel impossible.
Why Diets Fail - And What Actually Works
Ninety percent of people who lose weight through dieting regain it within five years. That’s not because they lack discipline. It’s because dieting triggers your body’s survival mode. When you cut calories, your metabolism slows down. Your hunger hormones spike. Your brain starts treating food like a scarce resource. This isn’t weakness - it’s evolution.
What works isn’t another diet. It’s long-term disease management. Think of it like high blood pressure or type 2 diabetes. You don’t cure it. You manage it. That means:
- Medical nutrition therapy from a dietitian certified in obesity care
- At least 150 minutes of moderate exercise per week - not to burn calories, but to improve insulin sensitivity and mood
- Behavioral counseling - 12 or more sessions - to address emotional eating, stress, sleep habits, and environmental triggers
- Medication, when appropriate
The most effective medications today are GLP-1 receptor agonists - drugs like semaglutide (Wegovy) and tirzepatide (Zepbound). In clinical trials, people lost 15 to 20% of their body weight over a year. That’s not magic. It’s biology. These drugs mimic a natural hormone that tells your brain you’re full. They reduce cravings, slow stomach emptying, and help stabilize blood sugar. Side effects? Nausea and digestive upset are common - about 65% of users report them. But for many, the trade-off is worth it.
And bariatric surgery? It’s not a last resort - it’s a proven treatment. Studies show it can lead to 25 to 35% weight loss and dramatically improve or even reverse type 2 diabetes. But it’s not simple. Forty-one percent of patients develop vitamin deficiencies. Twenty-nine percent experience dumping syndrome. And 37% say they didn’t get enough long-term support. That’s why surgery should only be done at centers that perform at least 125 procedures a year and offer lifelong follow-up care.

The Real Barriers to Treatment
Even with all this science, most people with obesity never get proper care. Only 7% of eligible U.S. adults receive guideline-recommended treatment. Why?
First, most doctors weren’t trained to treat obesity. Only 10% of U.S. medical schools require obesity education. Many still believe it’s a lifestyle issue. A 2023 survey found 69% of patients felt judged by their healthcare providers. Some were denied routine procedures like colonoscopies or knee replacements because of their weight.
Second, insurance won’t cover it. In 37 states, you need prior authorization just to get an obesity medication. Many plans won’t pay for dietitians, counseling, or even basic lab tests. Semaglutide can cost up to $1,400 a month without insurance. Even with coverage, copays can be $300 or more.
Third, there aren’t enough specialists. There are only about 1,200 dietitians in the U.S. with obesity certification. The country needs 35,000 more obesity medicine specialists to meet demand. That’s not a shortage - it’s a crisis.
What You Can Do Right Now
If you’re struggling with weight and metabolic health, here’s what actually helps - no gimmicks, no detoxes, no 30-day challenges:
- Ask your doctor for a full metabolic panel - check fasting insulin, liver enzymes, and HbA1c. These tell you more than your weight ever could.
- Request a referral to a registered dietitian with obesity certification. They don’t count calories. They help you build a sustainable eating pattern.
- Start moving - not to lose weight, but to feel better. A daily 20-minute walk reduces inflammation and improves sleep.
- Track your sleep. Aim for 7+ hours. Use a simple app if needed. Poor sleep is a silent driver of weight gain.
- Ask about medication. If you’ve tried everything and still can’t lose weight, ask if GLP-1 agonists or other FDA-approved treatments are right for you.
- Find support. Online communities like r/Obesity can help you feel less alone. But avoid groups that promote extreme diets or shaming.
Progress isn’t always visible on the scale. Sometimes, it’s sleeping better. Or needing less insulin. Or being able to climb stairs without getting winded. Those are wins. And they matter more than any number.

The Future Is Changing - But Slowly
There’s hope. The FDA approved retatrutide in 2023 - a triple-acting drug that showed 24.2% average weight loss in trials. New ICD-11 codes now classify obesity by stage and metabolic damage, not just BMI. The World Obesity Federation predicts nearly half the world’s population will have obesity by 2050. That’s not inevitable - but it will only change if we treat it like the disease it is.
For now, the best thing you can do is stop blaming yourself. Your body isn’t failing you. The system is. And you deserve care that matches the science - not the stigma.
Is obesity really a disease, or just a lifestyle problem?
Yes, obesity is officially recognized as a chronic disease by the American Medical Association, the World Health Organization, and major medical societies worldwide. It’s not caused by poor choices alone. It’s driven by complex biology - genetics, hormones, brain signaling, inflammation, and environmental factors. Treating it like a lifestyle issue ignores the science and leads to ineffective, harmful approaches.
Why do I keep gaining weight back after losing it?
Your body has powerful biological mechanisms to defend its weight. When you lose weight, your hunger hormones rise, your metabolism slows, and your brain becomes more focused on food. This isn’t weakness - it’s evolution. Studies show 90% of people regain most of their lost weight within five years, even with strict dieting. That’s why long-term medical management - not short-term diets - is needed.
Are weight-loss medications safe?
FDA-approved obesity medications like semaglutide and tirzepatide are safe for long-term use when prescribed correctly. They’ve been tested in large clinical trials lasting over a year. Common side effects include nausea and digestive discomfort, which usually improve over time. These drugs are not magic pills - they work best with lifestyle changes. But for many, they’re the first tool that actually helps them manage the disease.
Does bariatric surgery work long-term?
Yes, for many people, bariatric surgery leads to sustained weight loss and improvement in related conditions like type 2 diabetes and high blood pressure. Studies show 70-80% of patients maintain significant weight loss after five years. But it’s not without risks - vitamin deficiencies, dumping syndrome, and lack of long-term support are common. It requires lifelong follow-up and should only be done at accredited centers with comprehensive care teams.
Can I manage obesity without medication or surgery?
Some people can, especially in the early stages. Intensive behavioral therapy, medical nutrition counseling, and consistent physical activity can lead to meaningful health improvements - even without major weight loss. But for many, especially those with severe obesity or metabolic complications, these tools alone aren’t enough. That doesn’t mean failure. It means you need a more comprehensive approach - and you deserve one.
How do I find a doctor who treats obesity as a disease?
Look for providers certified by the Obesity Medicine Association (OMA) or endocrinologists with a focus on metabolic health. Ask directly: ‘Do you treat obesity as a chronic disease, and do you offer medications or referrals to dietitians and behavioral therapists?’ If they say ‘just eat less and exercise more,’ keep looking. You need a clinician who understands the biology, not the stigma.
Next Steps for Better Metabolic Health
If you’re ready to take action, start here:
- Book a visit with your primary care provider and ask for a metabolic panel.
- Search for an OMA-certified provider near you using the Obesity Medicine Association’s directory.
- Download a free sleep tracker app and aim for 7+ hours a night for two weeks.
- Start a daily 15-minute walk - no goal, no steps, no tracking. Just move.
- Write down one thing you’ve noticed about your body this month - not your weight, but how you feel, sleep, or move.
Healing isn’t about reaching a number. It’s about reclaiming your health - one real, sustainable step at a time.




Russell Thomas
December 30, 2025 AT 03:44