Most people have moles. Some are small, dark, and perfectly round. Others are raised, faded, or oddly shaped. The key question isn’t whether you have moles-it’s whether any of them might be dangerous. Melanoma, the deadliest form of skin cancer, doesn’t always look like the textbook example. That’s why the ABCDE rule exists: not as a final diagnosis, but as a simple, practical way to spot warning signs early.
What the ABCDE Rule Actually Means
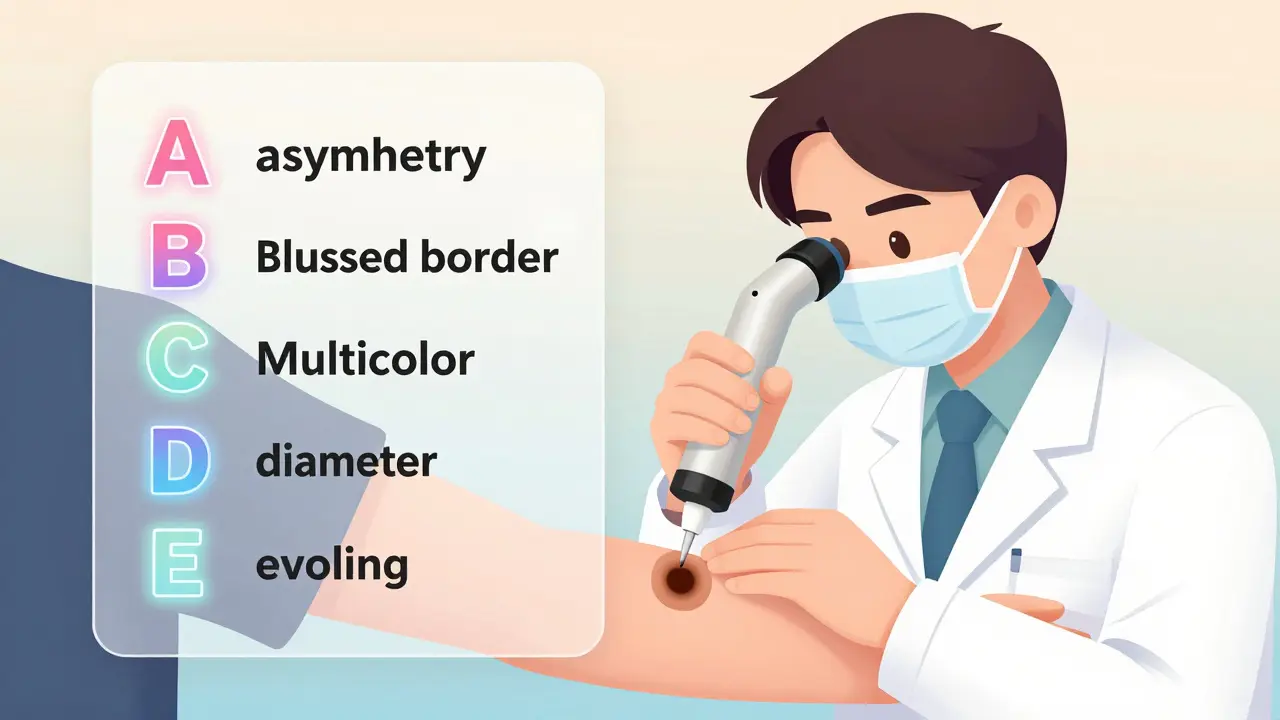
The ABCDE rule is a checklist used by dermatologists and patients alike to spot potential melanomas. It’s not perfect, but it’s the most widely taught tool for catching skin cancer before it spreads. Here’s what each letter stands for, and what it really means in practice:- A for Asymmetry: If you draw an imaginary line through the middle of the mole, both halves should match. If one side looks completely different from the other-like a lopsided blob-it’s a red flag.
- B for Border: Healthy moles have smooth, even edges. Melanomas often have jagged, blurred, or notched borders, like a stain bleeding through paper.
- C for Color: A normal mole is usually one shade of brown. A melanoma might have multiple colors: black, red, white, or blue mixed in. Even a single spot of unusual color, like a dark streak within a light mole, matters.
- D for Diameter: The old rule said 6 millimeters (about the size of a pencil eraser). But that’s outdated. Many melanomas are smaller than that. Some experts now say 5 mm is the real cutoff. More importantly, if a mole is darker than the others on your body, size doesn’t matter-it needs checking.
- E for Evolving: This is the most important sign. Any mole that changes over time-grows, bleeds, itches, crusts, or changes color-is suspicious. Even if it looks fine by ABCD standards, if it’s different from how it was six months ago, get it looked at.
Some clinics now use ABCDEFG, adding ‘F’ for ‘Funny looking’ and ‘G’ for ‘Growing rapidly.’ These aren’t official medical terms, but they reflect a real clinical insight: sometimes, a mole just feels wrong-even if it doesn’t tick every box.
Why the ABCDE Rule Misses So Many Melanomas
Here’s the uncomfortable truth: about one in three melanomas don’t follow the ABCDE rule at all. A 2022 study of 144 melanoma cases found that 36% were in situ-the earliest stage-yet only 33% showed the ‘E’ sign (evolving). Many were perfectly round, evenly colored, and smaller than 5 mm. One patient I read about had a melanoma that was only 3 mm wide, perfectly symmetrical, and had no color variation. It was stage IIB. No ABCDE criteria were met. But it was still cancer.Some melanoma types are especially sneaky. Desmoplastic melanoma, for example, often looks like a scar or a small bump with no color at all. Childhood melanomas rarely fit the pattern. In these cases, the ABCDE rule fails. That’s why dermatologists don’t rely on it alone.
The ‘Ugly Duckling’ Sign: A Better Clue Than ABCDE?
Think about your own skin. You probably have 10, 20, even 50 moles. Most of them look similar. One stands out-maybe darker, bigger, or just oddly shaped. That’s the ‘ugly duckling’ sign. It’s not in the ABCDE rule, but it’s often more reliable.A 2019 study in the British Journal of Dermatology found that the ugly duckling sign caught 73% of melanomas that ABCDE missed. Why? Because your body has a baseline. You know what your moles usually look like. If one suddenly looks like the odd one out, that’s a signal your brain picks up-even if you can’t explain why.
One Reddit user from Sydney described it this way: ‘I had 12 moles. Eleven looked like freckles. One looked like a tiny ink blot. I didn’t check ABCDE. I just thought, “That’s not mine.” I went in. It was melanoma.’
When Do You Need a Biopsy?
Not every weird-looking mole needs to be cut out. But some situations make a biopsy necessary:- Three or more ABCDE criteria are present
- The mole has changed noticeably over 3-6 months
- It’s the ugly duckling among your moles
- It’s bleeding, itching, or crusting without injury
- It’s darker than your other moles, even if small
Dermatologists use dermoscopy-a handheld magnifier with polarized light-to look deeper than the surface. In 85% of U.S. practices, this is standard. It boosts accuracy from 75% to 92%. But you don’t need one to know when to act. If you’re unsure, get it checked. No harm in being cautious.
Biopsies are quick. A local anesthetic numbs the area. The mole is removed with a small punch or shave tool. Results come back in 7-10 days. If it’s melanoma, catching it early means a 99% five-year survival rate. If it’s late-stage, that drops to 32%. That’s the difference between a routine follow-up and chemotherapy.
What’s Changing in Skin Cancer Screening?
The old way of screening everyone the same way is fading. The U.S. Preventive Services Task Force is updating its guidelines (expected in mid-2024) to focus on risk-not just appearance. People with fair skin, lots of moles, a family history of melanoma, or a history of sunburns will get more frequent checks. Others might not need annual full-body scans.Technology is catching up, too. AI tools like SkinVision, approved by the FDA in 2022, analyze photos of moles against a database of 12 million images. They’re 95% sensitive at spotting melanoma. But they’re not a replacement for a doctor-they’re a tool to help decide when to go in.
Some centers now use genetic tests like DecisionDx-Melanoma, which analyzes the mole’s DNA to predict if it’s dangerous. This can reduce unnecessary biopsies by 31%. But it’s expensive and not widely available outside major cities.
Why People Wait Too Long
A 2022 survey by the American Academy of Dermatology found that 42% of people who later got diagnosed with melanoma delayed seeing a doctor because their mole didn’t meet enough ABCDE criteria. They waited an average of 7.3 months. That’s long enough for a tiny melanoma to grow deeper and spread.One woman in Melbourne told her dermatologist: ‘I checked ABCDE. It wasn’t asymmetrical. No color change. Only 4 mm. I thought I was fine.’ Two months later, the mole was 8 mm, and it had spread to her lymph nodes. She needed a lymph node dissection. She didn’t need to lose that much time.
What You Should Do Now
You don’t need to be a doctor to protect yourself. Here’s what works:- Check your skin once a month. Use a mirror, or ask someone to help with your back.
- Look for the ugly duckling-the mole that doesn’t belong.
- Take a photo of any new or changing mole. Compare it in six months.
- If anything looks off-even if it doesn’t fit ABCDE-go to a dermatologist.
- Don’t wait for all five signs. One change is enough.
There’s no magic formula. But there’s a simple truth: early detection saves lives. Melanoma is treatable if caught early. It’s deadly if ignored. The ABCDE rule is a starting point-not the finish line.
Frequently Asked Questions
Can a mole be cancerous even if it’s small?
Yes. While melanomas are often larger than 6 mm, 30% are diagnosed when smaller than 5 mm. Size alone isn’t a reliable indicator. A small mole that’s changing color, bleeding, or looks different from your other moles should be checked.
Is the ABCDE rule still useful?
Yes, but not as a standalone tool. It’s a good starting point for spotting suspicious moles, especially in public awareness. But studies show it misses early melanomas, particularly in situ cases. Always combine it with the ‘ugly duckling’ sign and awareness of change over time.
How often should I get my moles checked by a doctor?
If you have no risk factors, a full-body skin check every 1-2 years is enough. If you have many moles, a history of sunburns, or a family history of melanoma, get checked annually. If you notice a changing mole, don’t wait-see a dermatologist right away.
Do I need a biopsy if my mole looks suspicious?
If a dermatologist suspects melanoma based on appearance, dermoscopy, or change over time, a biopsy is the only way to confirm. Most biopsies are minor procedures done in the office. The risk of spreading cancer from a biopsy is extremely low-far less than the risk of leaving it untreated.
Can I use phone apps to check my moles?
Apps like SkinVision can help you track changes and flag potential issues, but they’re not diagnostic tools. They’re best used to decide when to see a doctor. Never rely on an app to say ‘it’s fine.’ Always get professional evaluation for any changing or unusual mole.
What happens if melanoma is found?
If caught early (Stage 0 or I), the mole is removed with a small margin of healthy skin around it, and no further treatment is needed. If it’s deeper or has spread, you may need lymph node checks, immunotherapy, or targeted therapy. Survival rates drop sharply after Stage II, so early removal is critical.






Lily Steele
January 31, 2026 AT 12:08