When you switch from a brand-name drug to its generic version, do drug interactions change?
You’ve been taking your blood pressure pill for years. Your doctor switches you to the generic version to save money. Then you start feeling dizzy. You wonder: Is this because of the generic? Did the drug interaction with your other meds suddenly get worse?
It’s a common fear. But the science says something different.
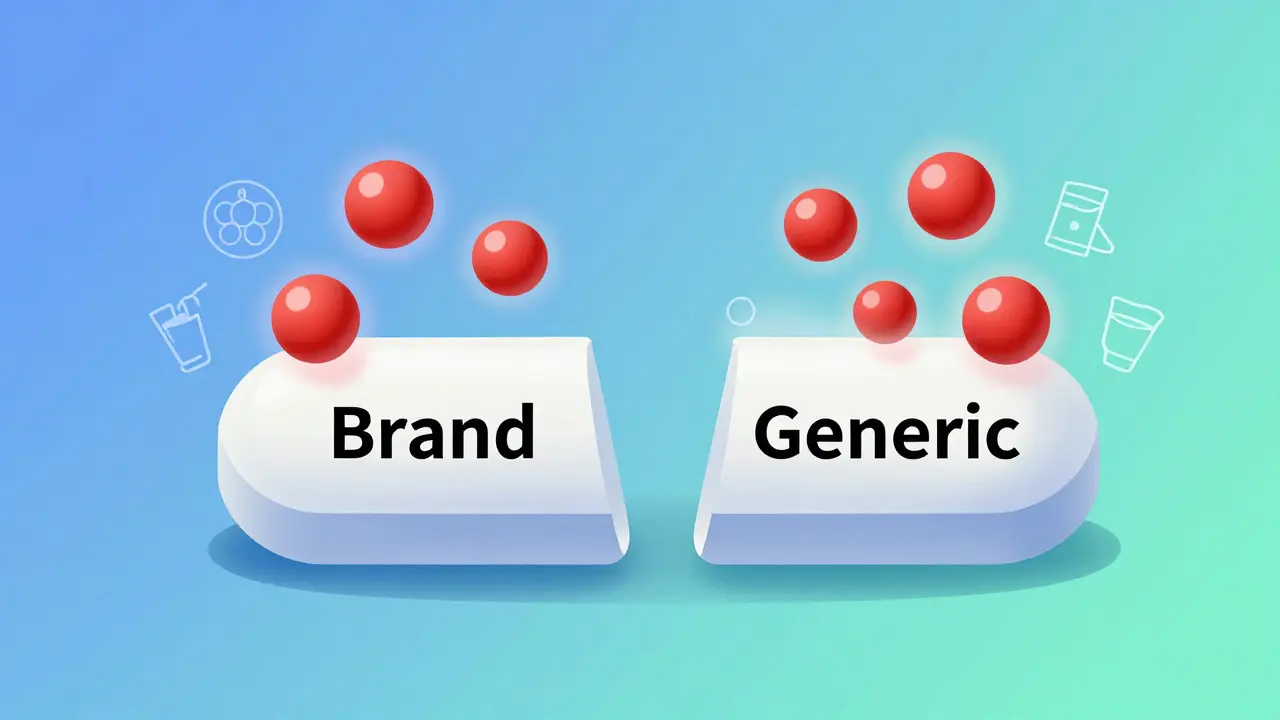
Generic drugs are not cheaper because they’re weaker. They’re cheaper because they don’t need to repeat the same expensive clinical trials that brand-name drugs did. The active ingredient-the part that actually works in your body-is identical. And so is the risk of drug interactions.
The U.S. Food and Drug Administration (FDA) requires every generic drug to prove it delivers the same amount of active medicine into your bloodstream at the same rate as the brand-name version. This is called bioequivalence. The standard allows for a small range: 80% to 125% of the brand’s absorption rate. That sounds wide, but in practice, most generics land within 5% of the original. For most drugs, that difference is meaningless.
Here’s the key point: drug interactions depend on the active ingredient, not whether the pill is made by Pfizer or Teva. If your medication interacts with grapefruit juice, alcohol, or another drug, that interaction stays the same whether it’s brand or generic. The chemistry doesn’t change.
What about the fillers and dyes? Can they cause different interactions?
Yes, but rarely-and not in the way most people think.
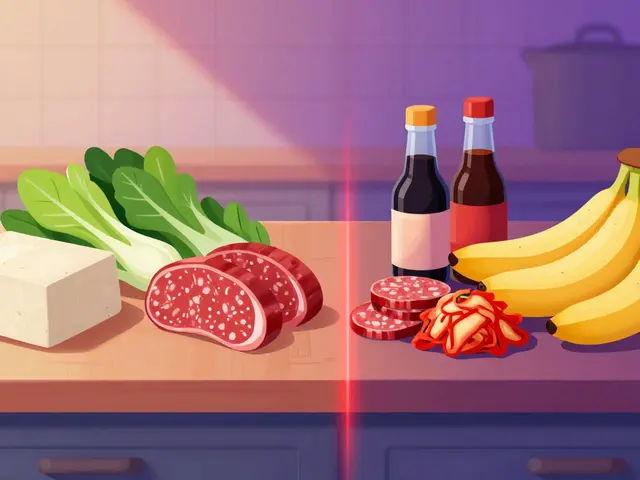
Generics can have different inactive ingredients: lactose, cornstarch, food dyes, preservatives. These don’t affect how the medicine works. But they can cause problems for people with allergies or intolerances.
For example, if you’re lactose intolerant and your brand-name pill uses lactose as a filler, but the generic uses rice starch, you might notice stomach upset. That’s not a drug interaction-it’s a reaction to the filler. The medicine itself still works the same way. Your blood pressure isn’t affected. Your liver isn’t processing the drug differently. You’re just reacting to something you’re allergic to.
The FDA now requires all approved generics to list their inactive ingredients in the Orange Book. Pharmacists can check this before filling your prescription. If you’ve had reactions to fillers before, tell your pharmacist. They can help you pick a version without the culprit ingredient.
And here’s something most people don’t realize: brand-name drugs also have fillers. They’re not pure active ingredient. They’re just more expensive fillers. The difference isn’t safety-it’s cost.
What about drugs with a narrow therapeutic index?
Some medicines have very little room for error. Too little, and they don’t work. Too much, and you get toxic side effects. These are called narrow therapeutic index (NTI) drugs. Examples include warfarin, levothyroxine, and some seizure medications.
For these, the FDA requires tighter bioequivalence standards: 90% to 111% instead of 80% to 125%. That means the generic must be much closer to the brand in how it’s absorbed.
Still, studies show no meaningful increase in adverse events when switching between generics or from brand to generic. A 2020 study in Scientific Reports looked at 17 NTI drugs and found that patients on generics had fewer heart attacks, strokes, and deaths than those on brand-name versions. That’s not because generics are better-it’s because people stick with generics longer. They’re cheaper, so patients take them consistently.
One real risk with NTI drugs is switching between different generics over time. Say you start with Generic A, then your pharmacy switches you to Generic B. If Generic A was at the low end of the bioequivalence range and Generic B is at the high end, your blood levels could shift slightly. That’s why doctors often recommend staying on the same generic version if possible. But even then, the change is usually small and manageable with monitoring.

Do people really experience different interactions with generics?
Yes. But it’s rarely because the drug itself changed.
On Reddit and WebMD, some users report new side effects after switching to a generic. Drowsiness. Headaches. Nausea. It feels real. But studies suggest this is often the nocebo effect-the opposite of placebo. If you believe generics are inferior, your brain might interpret normal side effects as something worse.
A 2022 Consumer Reports survey found that 18% of people thought generics had higher interaction risks. But only 4% actually experienced a change after switching. That gap tells you something: fear is louder than data.
One user on Reddit, ‘MedStudent2023,’ said switching from brand Ambien to generic zolpidem made them feel more drowsy when taking sertraline. But zolpidem is zolpidem. Sertraline is sertraline. The interaction between them doesn’t change because the pill looks different. What changed? Maybe the timing of the dose. Maybe they took it with food. Maybe they were stressed. The drug didn’t change. Their perception did.
What do experts say?
Dr. Aaron Kesselheim, a professor at Harvard Medical School, put it plainly: “The vast majority of evidence suggests that generic drugs are therapeutically equivalent to their brand-name counterparts, including regarding drug interaction profiles.”
The FDA’s Center for Drug Evaluation and Research says the same: inactive ingredients don’t alter how the drug interacts with other medicines. The American College of Clinical Pharmacology agrees.
There’s one exception: allergic reactions to fillers. That’s not a drug interaction-it’s an allergy. And it’s rare. Less than 1 in 1,000 patients report a true reaction to an inactive ingredient.
Even the most skeptical researchers agree: for 99% of prescriptions, switching to a generic doesn’t change your risk of interactions.
How do pharmacists handle this?
At UCSF Medical Center, pharmacists follow a simple rule: when a patient reports new side effects after switching to a generic, they check two things:
- Did the active ingredient change? (It didn’t.)
- Did the filler change? (Maybe.)
If the filler changed, they look up the new formulation in the FDA’s Orange Book. If it contains lactose, gluten, or a dye the patient is known to react to, they switch back or pick a different generic.
For most patients, though, the answer is simple: nothing changed. The interaction risk is the same. The medicine works the same. The side effects are the same.
Pharmacists also know that the biggest risk isn’t the generic-it’s stopping the medication because you think it’s “less safe.” That’s far more dangerous than any filler.
What about cost and compliance?
Let’s talk about the elephant in the room: money.
Generics save the U.S. healthcare system over $1.6 trillion in a decade. That’s real money. And that savings means people can afford their meds.
When people can’t afford their blood pressure pill, they skip doses. When they skip doses, their blood pressure spikes. That leads to strokes. That leads to hospital stays. That leads to death.
One study showed that patients on generics were more likely to take their meds regularly than those on brand-name versions. Why? Because they could afford them.
So if you’re worried about interactions, ask yourself this: Which is riskier-switching to a generic, or not taking your medicine at all?
Bottom line: The risk is the same
Drug interactions are about chemistry. Not branding.
The active ingredient in your generic is the same as in the brand. The way it interacts with other drugs, food, or supplements? Identical.
Yes, fillers can cause allergic reactions. But that’s not a drug interaction. It’s a food intolerance with a pill.
Yes, some people feel different after switching. But studies show it’s usually in their head-not their bloodstream.
For nearly every medication you take, the generic is just as safe, just as effective, and just as risky as the brand. The only real difference? The price tag.
If you’re concerned, talk to your pharmacist. Ask: “Is this generic the same as the brand?” They’ll show you the data. They’ll check the fillers. They’ll help you decide.
But don’t let fear stop you from saving money. Your body doesn’t know the difference. Your wallet does.


Shawn Peck
January 31, 2026 AT 02:29