Autoimmune uveitis isn’t just a red eye. It’s a silent threat to your vision, fueled by your own immune system turning against your eye. When the body mistakes parts of the uvea - the middle layer of the eye - as foreign invaders, it launches an inflammatory attack. This isn’t an infection you can treat with antibiotics. It’s an autoimmune war inside your eye, and if left unchecked, it can lead to cataracts, glaucoma, retinal detachment, or even permanent blindness. The good news? We now have ways to stop the damage without relying on steroids long-term.
What Happens When Your Immune System Attacks Your Eye
Uveitis means inflammation of the uvea, which includes the iris, ciliary body, and choroid. In autoimmune uveitis, this inflammation isn’t caused by bacteria or viruses. It’s triggered by your immune system attacking your own tissues. This can happen on its own, or it can be tied to bigger autoimmune diseases like ankylosing spondylitis, rheumatoid arthritis, lupus, Crohn’s disease, or sarcoidosis. About 10% to 20% of uveitis cases are linked to these systemic conditions, meaning your eye problem might be the first sign of something deeper.Symptoms don’t always come on fast. Some people notice blurry vision or floaters that slowly get worse. Others feel sharp pain, light sensitivity, or redness that hits suddenly. The inflammation can strike one eye or both. Left untreated, the constant swelling damages delicate structures inside the eye. Fluid builds up. Pressure rises. Scar tissue forms. Vision fades.
Why Steroids Are the First Line - and Why They Can’t Stay
When uveitis flares up, doctors reach for corticosteroids fast. Eye drops for front-of-the-eye inflammation. Injections near or inside the eye for deeper cases. Pills for widespread or severe disease. Steroids work because they’re powerful anti-inflammatories. They calm the immune system’s attack quickly.But here’s the catch: steroids are like a sledgehammer. They reduce inflammation, yes - but they also wreck other parts of your body over time. Long-term use raises your risk of cataracts, glaucoma, high blood pressure, weight gain, bone loss, and diabetes. For someone with chronic uveitis, taking steroids for months or years isn’t a solution. It’s trading one set of health problems for another.
That’s why steroid-sparing therapy isn’t optional. It’s essential. The goal isn’t to avoid steroids entirely - it’s to use them only as long as absolutely necessary, then switch to drugs that control the immune system without the same side effects.
Steroid-Sparing Therapies: The New Standard
Steroid-sparing therapy means using drugs that target the root cause - the overactive immune system - so you can reduce or stop steroids. These aren’t experimental. They’re backed by years of research and clinical use.Methotrexate is one of the oldest and most widely used. It’s an oral medication originally developed for cancer, but it’s been repurposed for autoimmune diseases for decades. It’s affordable, well-studied, and effective for many patients with chronic uveitis. But it takes weeks to kick in, and it needs regular blood tests to monitor liver and bone marrow function.
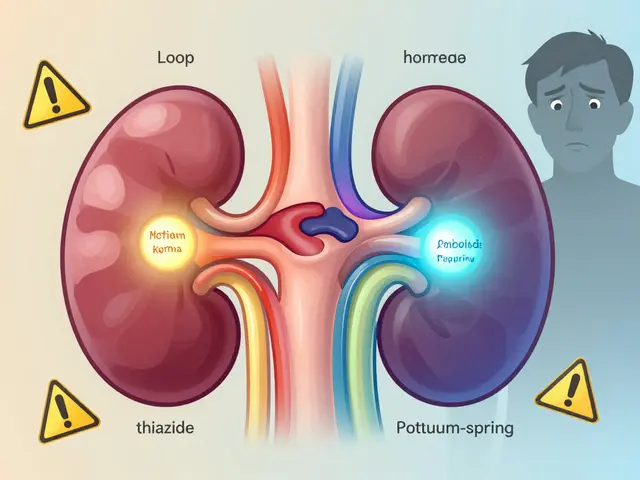
Cyclosporine is another immunosuppressant. It’s often used when methotrexate doesn’t work or isn’t tolerated. It can be taken orally or given as eye drops in some cases. The downside? It can affect kidney function and raise blood pressure, so close monitoring is required.
Then there are the biologics - targeted drugs that block specific parts of the immune response. The biggest breakthrough came in 2016, when the FDA approved Humira (adalimumab) for non-infectious uveitis. It’s a TNF-alpha inhibitor. TNF-alpha is a protein that drives inflammation in autoimmune diseases. By blocking it, Humira reduces eye swelling without the broad immune suppression of older drugs. It’s given as a weekly injection under the skin. Studies show it cuts steroid use by up to 70% in many patients.
Other biologics like infliximab have shown strong results, especially in kids with uveitis. Dr. Nisha Acharya’s research at UT Southwestern found that children on infliximab had dramatic improvements in vision and needed far less steroid support. These drugs are changing outcomes for people who used to lose vision despite treatment.

How Doctors Decide What’s Right for You
There’s no one-size-fits-all plan. Your treatment depends on:- Where the inflammation is - front, middle, back, or all of the eye
- How severe it is - mild flare or constant threat to vision?
- Whether you have another autoimmune disease
- How well you tolerated steroids
- Your overall health - liver, kidneys, infection history
Before starting any immunosuppressant, doctors run tests to rule out infections like tuberculosis or hepatitis. You can’t suppress your immune system if you have an active infection hiding in your body. Blood work, imaging like OCT scans, and sometimes fluorescein angiography help map the inflammation. A rheumatologist often works with your ophthalmologist because your eye disease might be a window into a larger condition.
For example, if you have uveitis and lower back pain, you might have ankylosing spondylitis. Treating the spine disease often helps the eye too. That’s why collaboration between specialists isn’t just helpful - it’s necessary.
What to Expect When You Start Steroid-Sparing Therapy
Switching from steroids to immunosuppressants isn’t instant. It takes time - sometimes months - for these drugs to build up in your system and fully control inflammation. During that transition, you might still need low-dose steroids to keep symptoms in check. That’s normal.Side effects vary. Methotrexate can cause nausea or fatigue. Biologics like Humira increase your risk of infections - colds, sinus infections, even rare ones like tuberculosis. You’ll need regular check-ups: blood tests every few weeks, eye exams every 1-3 months, and monitoring for signs of new infections.
Many patients report better quality of life after switching. No more moon face. No more sugar cravings. No more sleepless nights worrying about cataracts. But you do trade one set of risks for another. The key is balance: enough suppression to protect your vision, not so much that you’re constantly sick.
The Future: Personalized Treatment Is Coming
Right now, choosing the right steroid-sparing drug feels a bit like trial and error. But that’s changing. Researchers are studying biomarkers - tiny signals in your blood or genes - that might predict which drug will work best for you. Are you more likely to respond to a TNF blocker? Or would an interleukin inhibitor like secukinumab work better? Clinical trials are testing drugs targeting IL-6, IL-17, and JAK pathways, with early results showing promise for patients who don’t respond to Humira.Specialized uveitis clinics have grown from just 15 in 2010 to over 50 across the U.S. today. These centers bring together ophthalmologists, rheumatologists, and pharmacists who see these cases every day. They’re the ones pushing the field forward.
For now, the message is clear: if you have autoimmune uveitis, you don’t have to live on steroids forever. There are better, safer options. The key is starting the conversation early - with your eye doctor, and with a specialist who understands the full picture.
When to Seek Help
Don’t wait. If you notice:- Sudden blurred vision
- Eye pain or redness that doesn’t go away
- Floaters that increase
- Sensitivity to light
Get seen by an ophthalmologist within 24 hours. Delaying treatment increases the risk of permanent damage. If you’ve already been diagnosed with uveitis and your symptoms are returning, don’t just reach for your steroid drops again. Talk to your doctor about steroid-sparing options. Your vision is worth more than a quick fix.
Is autoimmune uveitis the same as regular eye inflammation?
No. Regular eye inflammation can be caused by infection, injury, or irritation. Autoimmune uveitis happens when your immune system attacks your eye tissue without an external trigger. It’s chronic, often recurrent, and linked to systemic autoimmune diseases. Treatment is completely different - antibiotics won’t help, but immunosuppressants might.
Can I stop steroids once I start steroid-sparing therapy?
Yes, but not right away. Steroid-sparing drugs take weeks to months to work. Your doctor will slowly reduce your steroid dose while monitoring your eye closely. Stopping steroids too fast can cause a flare. The goal is to reach the lowest possible dose - or none at all - while keeping inflammation under control.
Are biologics like Humira safe for long-term use?
They’re safer than long-term steroids, but not risk-free. Biologics increase your chance of infections, including serious ones like TB or fungal infections. You’ll need screening before starting and regular check-ups while on them. Most people tolerate them well, especially compared to the damage steroids cause over time. For many, the benefits far outweigh the risks.
Why do I need to see a rheumatologist if my problem is my eye?
Autoimmune uveitis is often a sign of a larger autoimmune condition - like lupus, Crohn’s, or ankylosing spondylitis. A rheumatologist can test for these, treat the root cause, and help choose the best immunosuppressant. Treating your eye alone without addressing the systemic disease often leads to repeat flares. Team-based care gives you the best shot at long-term vision protection.
What if steroid-sparing therapy doesn’t work?
There are other options. Newer drugs targeting different immune pathways - like IL-17 or JAK inhibitors - are being tested in clinical trials. Some patients respond better to combinations of drugs. Surgery might be needed for complications like cataracts or glaucoma, but the goal is always to control the inflammation first. Don’t give up - there’s almost always another option.
Next Steps: What You Can Do Today
- If you have uveitis and are on steroids, ask your doctor if you’re a candidate for steroid-sparing therapy.
- Get screened for underlying autoimmune conditions - blood tests can reveal hidden links.
- Find a uveitis specialist or a clinic with both ophthalmology and rheumatology teams.
- Keep a symptom journal - note changes in vision, pain, or fatigue. This helps your doctor adjust treatment.
- Don’t skip follow-ups. Even if you feel fine, inflammation can be quietly damaging your eye.
Autoimmune uveitis doesn’t have to mean losing your sight. With the right treatment plan - one that moves beyond steroids - you can protect your vision and live well. The tools are here. You just need to ask for them.





Jim Oliver
November 10, 2025 AT 17:53