Top 7 Wellbutrin Sr Alternatives in 2025: A Comprehensive Guide
January 27 2025Hepatic Encephalopathy: What You Need to Know
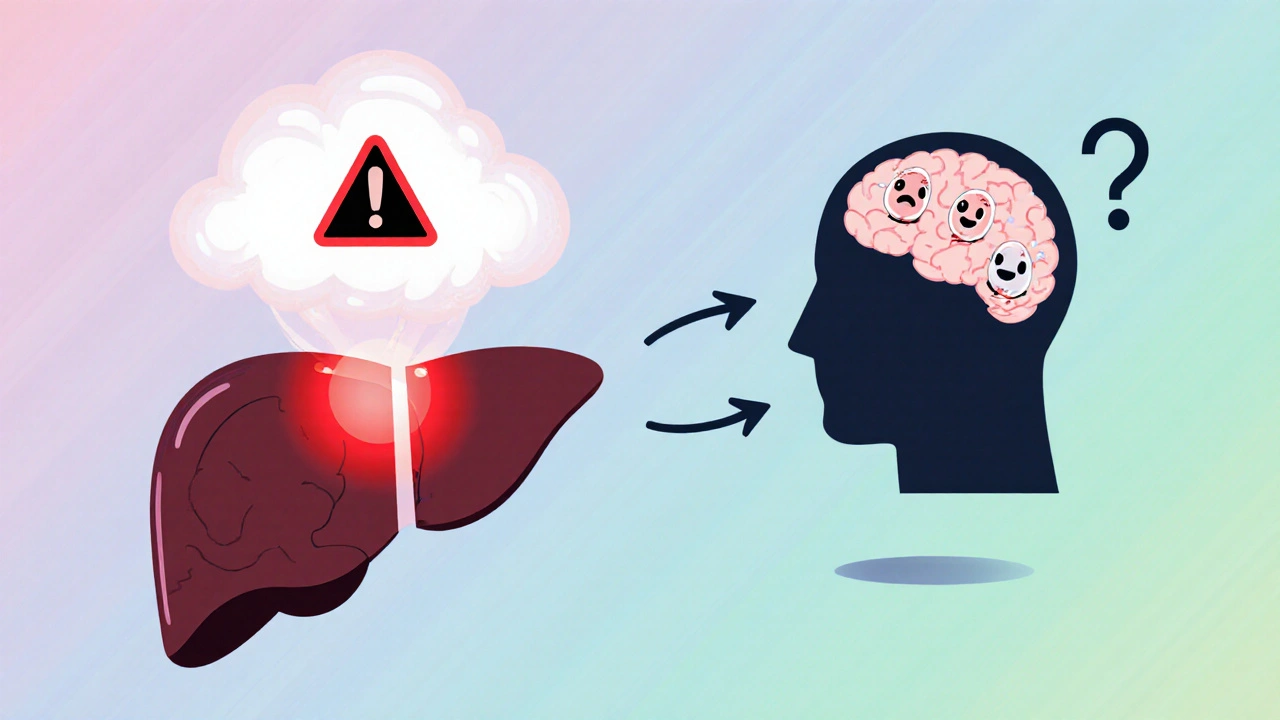
When dealing with hepatic encephalopathy, a neuropsychiatric syndrome that arises from severe liver dysfunction and toxin accumulation. Also known as HE, it often manifests as confusion, altered sleep patterns, and motor disturbances. Liver disease includes conditions like cirrhosis and hepatitis that impair the organ’s detoxifying ability creates the perfect storm for ammonia a waste product normally converted to urea by a healthy liver to flood the bloodstream. Elevated blood ammonia then crosses the blood‑brain barrier, disrupting neurotransmission and leading to the hallmark signs of hepatic encephalopathy. Managing this condition hinges on reducing ammonia levels and supporting liver function, which is where medications such as lactulose a non‑absorbable sugar that traps ammonia in the gut and rifaximin an antibiotic that lowers gut bacteria producing ammonia become essential tools.
Key Factors and Management Strategies
Understanding hepatic encephalopathy starts with recognizing its triggers. Common precipitants include gastrointestinal bleeding, infections, constipation, and excessive dietary protein. Each of these can spike ammonia production or reduce its clearance. For instance, a bleed in the stomach releases blood proteins that gut bacteria break down into ammonia, aggravating brain toxicity. Therefore, early identification of bleeding sources and prompt endoscopic or pharmacologic treatment can prevent an HE flare. Effective treatment typically follows a two‑step approach: first, quickly lower ammonia using lactulose (often started at 25 ml three times daily and titrated to achieve 2–3 soft stools per day); second, add rifaximin 550 mg twice daily for patients with recurrent episodes or those who do not fully respond to lactulose alone. This combination has been shown to cut hospitalization rates and improve quality of life.
Beyond medication, lifestyle adjustments play a major role. Patients should maintain a moderate protein intake—enough to prevent malnutrition but not so high as to overload the liver's detox capacity. Small, frequent meals with protein spread throughout the day help keep blood ammonia stable. Hydration is another simple yet powerful tactic; adequate fluid intake supports kidney function, which also removes nitrogenous waste. Moreover, avoiding sedatives, alcohol, and over‑the‑counter supplements that strain liver metabolism can reduce the risk of episodes. Coordination with a dietitian experienced in liver disease ensures personalized plans that respect cultural preferences while meeting nutritional needs.
Finally, regular monitoring is vital. Routine blood tests for ammonia, liver enzymes, and coagulation profiles give clinicians a snapshot of disease progression. Cognitive assessments, such as the number‑connection test, help track subtle changes in mental status before they become obvious. When a patient presents with new confusion, a quick bedside screen can differentiate HE from other causes like infection or electrolyte imbalance. The collection of articles below dives deeper into each of these topics—from medication comparisons and dosing nuances to lifestyle tips and when to seek emergency care—giving you a complete toolbox to manage hepatic encephalopathy effectively.
 20 Oct
20 Oct
Probiotics for Hepatic Encephalopathy: Treatment Insights
Learn how probiotics can aid hepatic encephalopathy treatment, from the science behind gut‑liver interaction to practical tips and clinical evidence for patients and caregivers.
Read More...




