Erosive Esophagitis and Anxiety: How They're Connected and What to Do
July 1 2023Drug interactions: how to spot and avoid risky combinations
One pill can change how another works — and sometimes that change is dangerous. Drug interactions happen when medicines, supplements, or foods alter a drug’s effect. Some interactions make a drug weaker, others push levels so high you get bad side effects. Knowing the common patterns helps you avoid harm and unnecessary trips to the ER.
There are three common types: drug‑drug (two or more medicines), drug‑food (grapefruit is the famous one), and drug‑supplement (herbs, vitamins, or over‑the‑counter products). For example, some antibiotics raise warfarin levels and increase bleeding risk. Grapefruit juice can boost certain statins and cause muscle pain. St. John’s wort can lower many antidepressants and birth control effectiveness. These aren’t rare surprises — they’re predictable if you know what to watch for.
Quick rules to avoid interactions
Keep a single, up‑to‑date list of everything you take: prescriptions, OTC drugs, vitamins, and herbal supplements. Bring that list to every medical visit and pharmacy. Use one pharmacy when possible—pharmacists can spot dangerous combos when they fill multiple prescriptions for you. Read medication leaflets for interaction warnings and follow timing instructions (some drugs must be taken hours apart).
Watch out for common danger signs: mixing blood thinners with NSAIDs raises bleeding risk; combining SSRIs with certain migraine meds can increase serotonin effects; and mixing cholesterol drugs with grapefruit may cause muscle damage. If you take medicines like warfarin, atorvastatin, sertraline, or blood thinners such as apixaban, be extra cautious—these show up often in interaction reports.
Tools and when to ask for help
Use interaction checkers from trusted sources or ask your pharmacist to run a check. Apps like pharmacy discount tools sometimes include interaction warnings, but always double‑check with a clinician. Before starting a new OTC pain reliever, supplement, or travel vaccine, ask if it will affect your current meds. If you notice sudden dizziness, severe stomach pain, unusual bleeding, muscle weakness, or extreme drowsiness after starting a new drug, contact your doctor or pharmacist right away.
Travelers: plan ahead. Time zone changes, storage issues, and schedule shifts can affect how you take meds. If you’re on critical drugs (anticoagulants, heart meds, psychiatric meds), get a written plan from your prescriber and carry enough supply with original labels.
Practical habit to start today: keep a photo of your medication list on your phone, always show it at medical visits, and ask the pharmacist one clear question when you pick up a new drug — “Does this interact with what I already take?” That simple step prevents most surprises.
 21 Feb
21 Feb
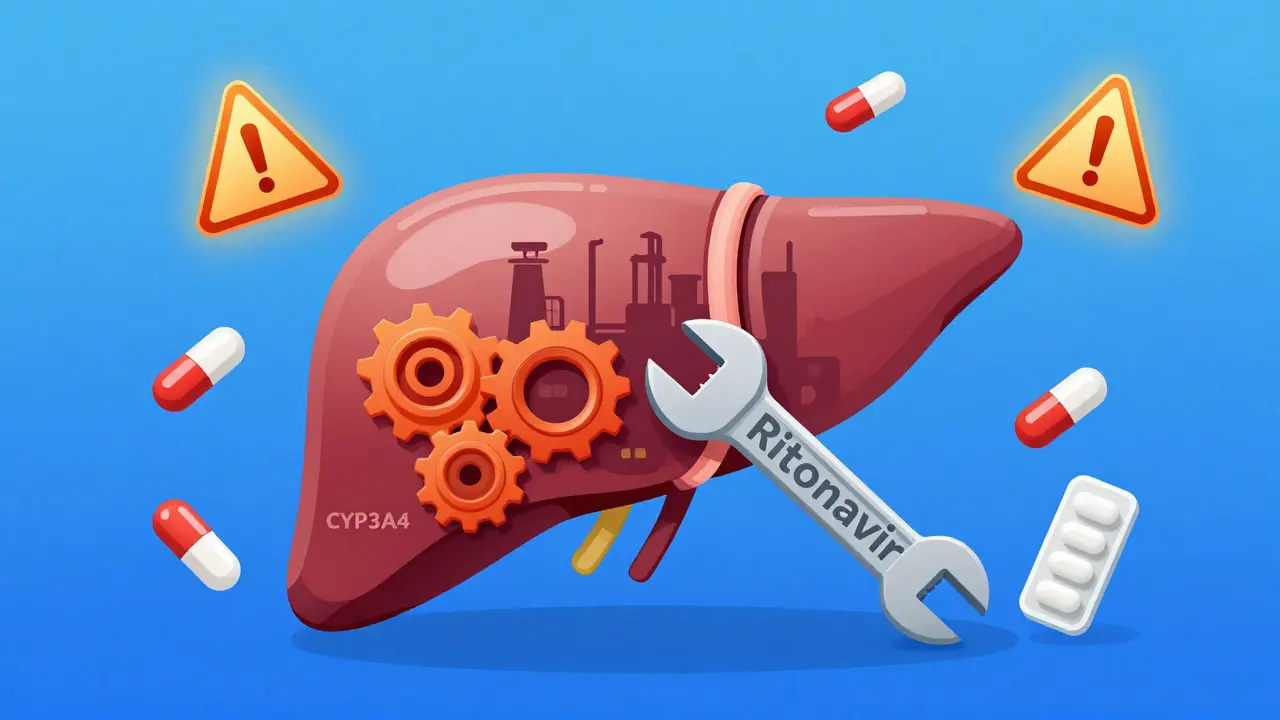
Lopinavir/Ritonavir Boosting: How CYP3A4 Interactions Shape Drug Safety and Treatment Outcomes
Lopinavir/ritonavir boosting relies on CYP3A4 inhibition to maintain HIV drug levels-but this mechanism triggers dangerous interactions with over 1,200 other medications. Learn how it affects statins, blood thinners, anesthesia, and birth control-and why it's still used despite safer alternatives.
Read More... 30 Jan
30 Jan
Drug Interactions: Same Risk for Generic and Brand Medications
Generic and brand-name drugs have the same active ingredients, so their risk for drug interactions is identical. Learn what really changes-and what doesn't-when you switch from brand to generic.
Read More...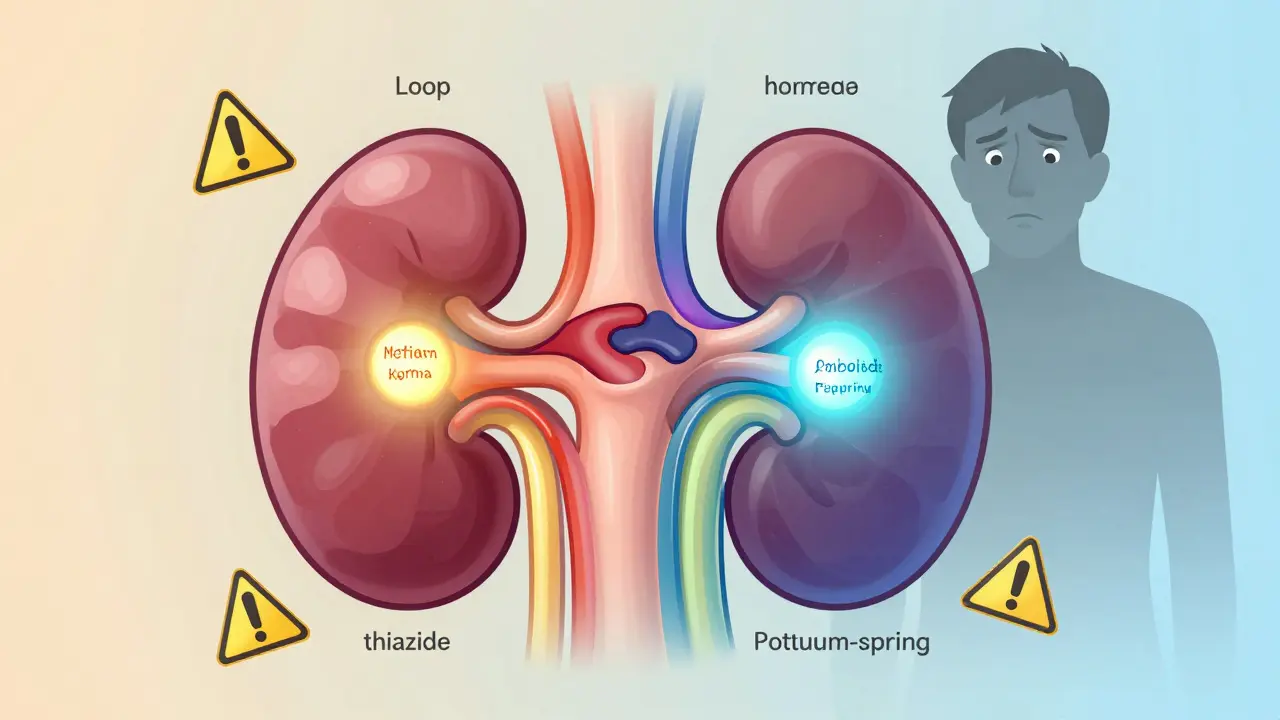 27 Dec
27 Dec
Diuretics: Understanding Electrolyte Changes and Dangerous Drug Interactions
Diuretics help manage fluid buildup and high blood pressure, but they can cause dangerous electrolyte shifts and harmful drug interactions. Learn how loop, thiazide, and potassium-sparing diuretics affect sodium and potassium - and how to stay safe.
Read More... 30 Oct
30 Oct
Motion Sickness Medications: Scopolamine and Sedative Interactions
Scopolamine patches are the most effective treatment for motion sickness, but they cause strong drowsiness and can become dangerous when mixed with alcohol, sedatives, or CBD. Learn how to use them safely and avoid life-threatening interactions.
Read More... 23 Feb
23 Feb
Dosulepin and ECT: Unpacking Potential Interactions
Exploring the interaction between Dosulepin, a traditional antidepressant, and Electroconvulsive Therapy (ECT), a significant treatment for severe depression. Learn about the ways these treatments might affect each other, their use in psychiatry, and things to consider before combining them. This article aims to simplify and clarify the complexities for better patient care.
Read More...