Diuretics are one of the most commonly prescribed drug classes in the world, especially for managing high blood pressure, heart failure, and fluid buildup. But behind their effectiveness lies a hidden risk: electrolyte changes and drug interactions that can turn a safe treatment into a medical emergency. Many people take these pills without realizing how easily their potassium, sodium, or magnesium levels can swing out of range - sometimes with deadly results.
How Diuretics Work - And Why They Disrupt Your Body’s Balance
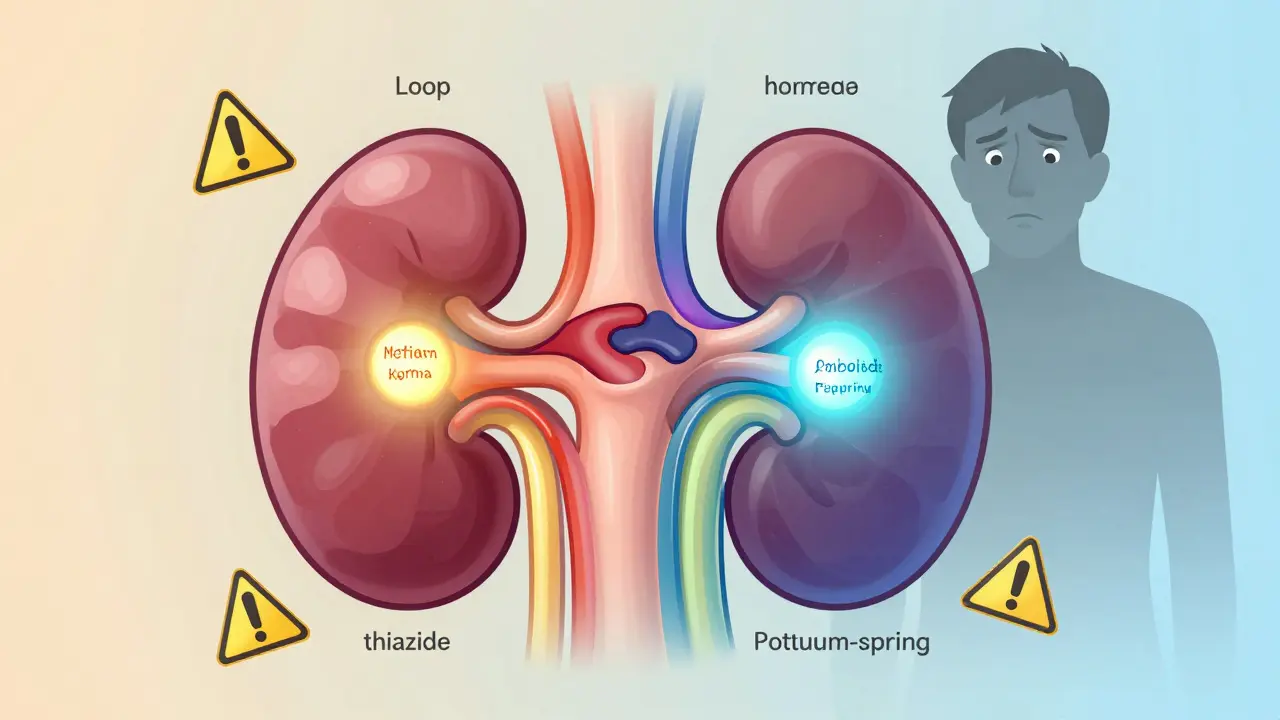
Diuretics don’t just make you pee more. They work by blocking specific sodium channels in your kidneys, forcing your body to flush out salt and water. But sodium doesn’t travel alone. It drags other electrolytes like potassium, chloride, and magnesium with it. The exact effect depends on which part of the kidney the drug targets.Loop diuretics like furosemide and bumetanide act high up in the loop of Henle. They’re powerful - they can push out 20-25% of filtered sodium. That’s why they’re used in heart failure or severe swelling. But this power comes at a cost: they cause big drops in potassium and magnesium, and surprisingly, they can even raise sodium levels in some cases by removing too much water relative to salt.
Thiazide diuretics like hydrochlorothiazide work lower down, in the distal tubule. They’re gentler, removing only 5-7% of sodium. That’s why they’re first-line for high blood pressure. But they’re notorious for causing hyponatremia - low sodium - especially in older women. Their slow, steady action makes them good for daily use, but they’re dangerous if you’re dehydrated or on other meds that affect sodium.
Potassium-sparing diuretics like spironolactone and amiloride work in the collecting duct. They block aldosterone, the hormone that tells your kidneys to hold onto salt and dump potassium. So they keep potassium in - great, right? But if you’re already taking an ACE inhibitor or have kidney trouble, this can push your potassium too high. A level above 5.5 mmol/L can trigger cardiac arrest.
The Real Danger: Electrolyte Crashes You Can’t Afford to Ignore
A 2013 study of 20,000 ER patients found that 3% were on multiple diuretics. Nearly half of them had dangerous electrolyte shifts. These aren’t just lab numbers - they’re life-or-death events.Hyponatremia (sodium under 135 mmol/L) from thiazides can cause confusion, seizures, and coma. It’s especially common in elderly women taking hydrochlorothiazide for hypertension. One patient I read about - a 78-year-old woman on 25mg of HCTZ - collapsed after a week of mild diarrhea. Her sodium was 121. She spent three days in the ICU.
Hypokalemia (potassium under 3.5 mmol/L) from loop or thiazide diuretics leads to muscle cramps, irregular heartbeat, and sudden cardiac events. In a 2022 case report, a 65-year-old man on furosemide for heart failure had a cardiac arrest after switching to a new generic brand. His potassium dropped from 4.1 to 2.9 in 48 hours. The generic had less consistent absorption - a small change, with huge consequences.
Hyperkalemia (potassium over 5.0 mmol/L) from spironolactone is equally terrifying. A 2023 Reddit thread from a nurse described a patient on 50mg of spironolactone who started Bactrim (trimethoprim-sulfamethoxazole) for a UTI. Three days later, his potassium hit 6.8. He needed emergency dialysis. The antibiotic blocks potassium excretion - a known interaction, but still routinely missed.
These aren’t rare. The European Medicines Agency found that 14.3% of heart failure patients on spironolactone developed potassium levels above 5.5 mmol/L - nearly 1 in 7. And the risk spikes when you combine drugs.
Drug Interactions: When Your Meds Fight Each Other
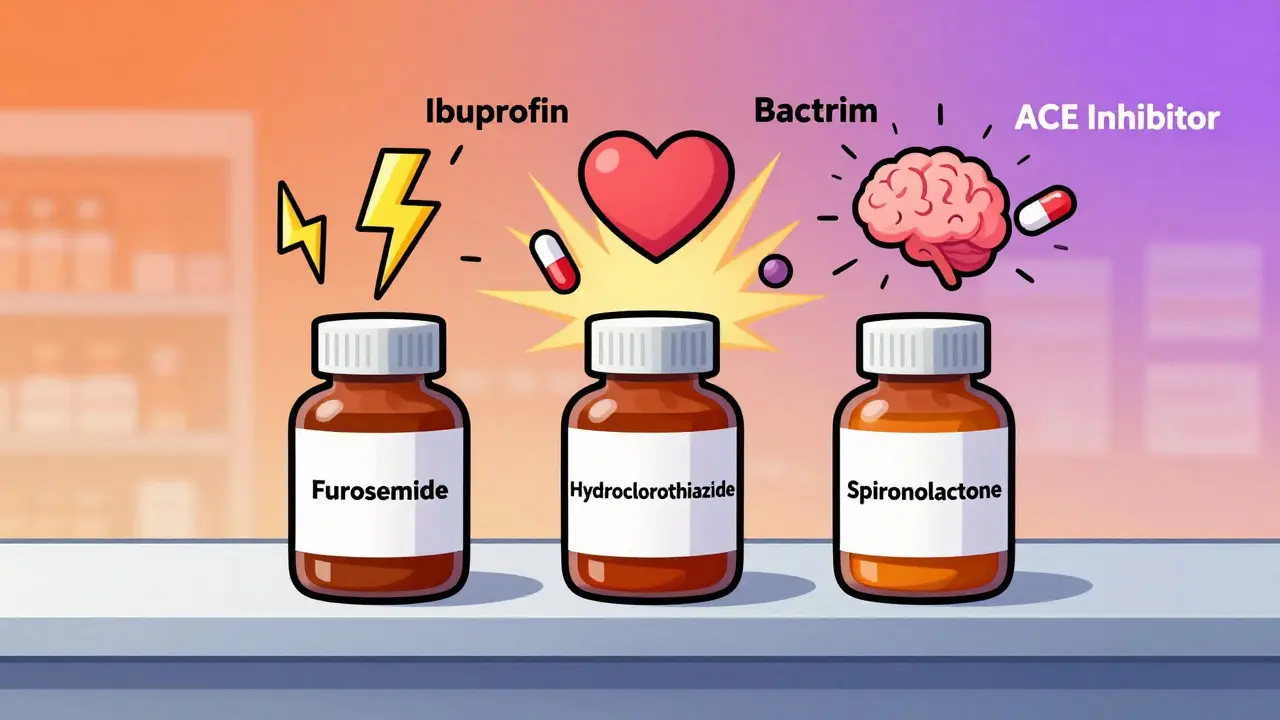
Diuretics don’t live in isolation. They’re often stacked with other drugs - and that’s where things go wrong.NSAIDs like ibuprofen or naproxen are a major red flag. They cut diuretic effectiveness by 30-50%. Why? They block prostaglandins, which help keep blood flowing to your kidneys. Without that, your kidneys can’t respond to the diuretic. A patient on furosemide for leg swelling might take Advil for arthritis - and wonder why the swelling got worse.
ACE inhibitors and ARBs are another double-edged sword. They help heart failure patients live longer. But when paired with spironolactone, they can push potassium into the danger zone. A 2019 meta-analysis showed this combo raised potassium by 1.2 mmol/L - more than double the rise from either drug alone. That’s why guidelines demand weekly potassium checks when starting this combination.
Then there’s the new player: SGLT2 inhibitors like dapagliflozin. Originally for diabetes, they’re now used in heart failure. They work by making the kidneys dump glucose and sodium. But when you add them to a loop diuretic, something unexpected happens: the diuretic’s effect jumps by nearly 200%. Why? The SGLT2 inhibitor reduces sodium reabsorption early in the kidney, leaving more for the loop diuretic to act on. This synergy is powerful - but it can cause severe dehydration or kidney injury if not managed carefully.
Even antibiotics can be dangerous. Trimethoprim (in Bactrim) acts like a potassium-sparing diuretic. Add it to spironolactone, and you’re stacking two potassium-retaining drugs. One case in the American Journal of Medicine described a patient who went from a normal potassium of 4.3 to 6.1 in just 72 hours after starting Bactrim. He didn’t have kidney disease. He didn’t have diabetes. He just took two common drugs together.
Combining Diuretics: When More Is Not Better
Doctors sometimes combine diuretics to overcome resistance - when the body starts holding onto sodium again after a few days of treatment. The classic combo is furosemide (loop) plus metolazone (thiazide). It’s effective: the DOSE trial showed 68% of patients responded versus 32% on loop alone.But it’s risky. A 2017 study found 22% of patients on this combo developed acute kidney injury. Another 15% got dangerously low sodium. Why? You’re hitting two different parts of the kidney at once. Your body can’t compensate. You’re flushing out too much fluid, too fast.
Triple therapy - loop, thiazide, and potassium-sparing - is even more dangerous. A 2024 meta-analysis found patients on this regimen had more than double the risk of acute kidney injury. Yet, 31% of hospitalized heart failure patients still get this combo. It’s often done out of desperation, not strategy.
The smarter approach? Match the drug to the problem. If your kidney function is poor (eGFR under 30), use loop diuretics. If it’s normal, thiazides are safer. If you’re losing potassium, add a potassium-sparing - but only if you’re not on an ACE inhibitor and your kidneys are working well. And never start a new combo without checking electrolytes within 3-7 days.

Monitoring: The Only Way to Stay Safe
There’s no magic pill that avoids electrolyte problems. The only protection is vigilance.Guidelines say: check your electrolytes within 3-7 days of starting any diuretic. Then every 1-3 months if you’re stable. But if you’re changing doses, adding a new drug, or feeling weak or dizzy - check sooner. Many patients don’t realize their symptoms are tied to their meds until it’s too late.
Some hospitals now use automated alerts. Johns Hopkins reduced hyponatremia by 37% and hyperkalemia by 29% over 18 months by setting up electronic flags when a diuretic was prescribed with an ACE inhibitor or NSAID. The system nudged doctors to order labs before the patient left the clinic.
Even simple habits help. If you’re on a thiazide, avoid salt substitutes - they’re full of potassium. If you’re on spironolactone, don’t eat large amounts of potassium-rich foods like bananas, oranges, or spinach without checking with your doctor. And never skip your blood tests because you “feel fine.” Electrolyte crashes don’t always come with warning signs.
The Future: Smarter Diuretics, Fewer Risks
The field is changing. In January 2024, the FDA approved Diurex-Combo - a single pill with furosemide and spironolactone. Early data from the DIURETIC-HF trial showed it cut 30-day heart failure readmissions by 22% and reduced electrolyte emergencies by more than half.Meanwhile, SGLT2 inhibitors are becoming standard add-ons for heart failure. They’re not diuretics, but they make diuretics work better - with less risk of potassium loss. The 2023 ACC/AHA guidelines now recommend them alongside loop diuretics for patients with reduced heart function.
Looking ahead, AI-driven dosing tools are being tested. Mayo Clinic’s pilot program used patient data - age, kidney function, meds, recent labs - to predict the safest diuretic dose. It reduced electrolyte emergencies by 40% in six months. These tools won’t replace doctors, but they’ll help prevent the mistakes that still happen every day.
Diuretics are essential. They save lives. But they’re not harmless. Their power comes with precision. The right drug, the right dose, the right monitoring - that’s the difference between recovery and crisis.
Can diuretics cause low sodium? What are the signs?
Yes, especially thiazide diuretics like hydrochlorothiazide. They impair the kidney’s ability to dilute urine, leading to hyponatremia (sodium under 135 mmol/L). Signs include confusion, nausea, headache, muscle weakness, and in severe cases, seizures or coma. Elderly women are at highest risk, especially if dehydrated or taking NSAIDs.
Is it safe to take ibuprofen with a diuretic?
No, it’s not safe. NSAIDs like ibuprofen reduce blood flow to the kidneys by blocking prostaglandins. This cuts diuretic effectiveness by 30-50% and increases the risk of kidney injury. If you need pain relief, talk to your doctor about alternatives like acetaminophen.
Why does spironolactone raise potassium levels?
Spironolactone blocks aldosterone, a hormone that tells your kidneys to get rid of potassium. Without aldosterone, potassium builds up in your blood. This is intentional - it prevents low potassium from other diuretics. But if you also take an ACE inhibitor or have kidney disease, potassium can rise dangerously high, leading to heart rhythm problems.
Can I take potassium supplements with my diuretic?
Only if your doctor says so. If you’re on a loop or thiazide diuretic, your doctor may prescribe potassium supplements to prevent low levels. But if you’re on a potassium-sparing diuretic like spironolactone, supplements can cause life-threatening high potassium. Never take them without a blood test and medical approval.
What should I do if I miss a dose of my diuretic?
Take it as soon as you remember, unless it’s close to your next dose. Don’t double up. Missing a dose won’t cause immediate danger, but it can lead to fluid buildup over time. If you miss multiple doses and feel swollen, short of breath, or gain weight rapidly, contact your doctor - you may need a dose adjustment or lab check.
Are there natural alternatives to diuretics?
Some foods and herbs like dandelion, green tea, and celery seed have mild diuretic effects. But they’re not strong enough to treat heart failure, high blood pressure, or severe swelling. They also interact with medications and can worsen electrolyte imbalances. Don’t replace prescribed diuretics with natural options without medical advice.
How often should I get my electrolytes checked on diuretics?
Within 3-7 days after starting or changing your dose. Then every 1-3 months if stable. If you’re on multiple diuretics, an ACE inhibitor, or have kidney disease, check every 2-4 weeks. Always get tested before starting new medications like antibiotics or NSAIDs.
Can diuretics damage my kidneys?
They don’t damage kidneys directly, but they can cause acute kidney injury if you’re dehydrated, on NSAIDs, or taking too high a dose. This is especially true with combination therapy (like loop + thiazide). Always stay hydrated, avoid NSAIDs, and get regular blood tests to monitor kidney function.




Gerald Tardif
December 28, 2025 AT 01:18