For millions of people worldwide, stomach pain, bloating, and erratic bowel habits aren’t just inconvenient-they’re life-limiting. If you’ve been told your symptoms are "just stress" or "all in your head," you’re not alone. But here’s the truth: irritable bowel syndrome isn’t a mental health issue disguised as a gut problem. It’s a real, measurable breakdown in communication between your gut and your brain. And understanding that connection is the key to real relief.
What IBS Really Is (And What It Isn’t)
IBS isn’t an infection, a tumor, or inflammation. It doesn’t show up on a colonoscopy or blood test. That’s why it’s been misunderstood for decades. The Rome IV criteria, used by doctors since 2016, define IBS by three things: recurrent belly pain at least once a week for three months, plus two of these: pain linked to bowel movements, changes in stool frequency, or changes in stool appearance. But here’s what most doctors don’t tell you: 76% of people with IBS also have constant, non-painful discomfort. Nearly two out of three also struggle with anxiety or depression-not because they’re weak, but because their nervous system is stuck in overdrive.
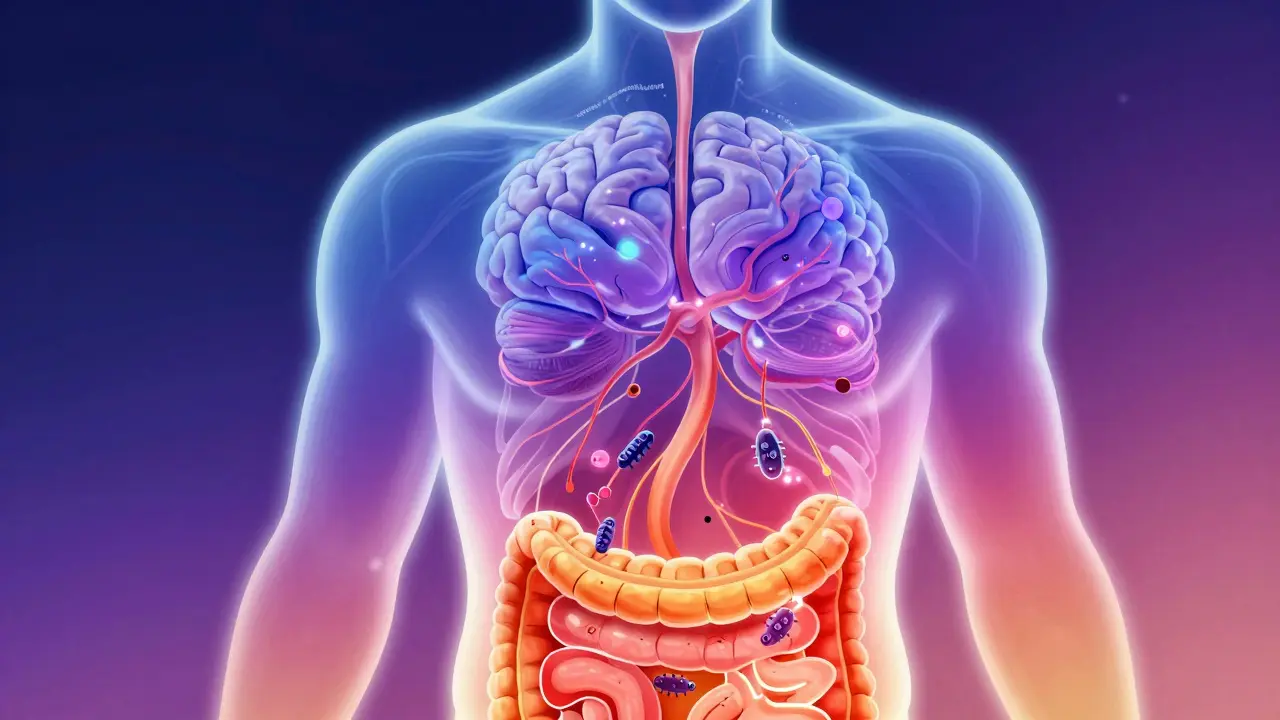
For years, IBS was seen as a problem with gut motility-too fast, too slow. But research since 2020 has flipped that idea. We now know IBS is a disorder of brain-gut-microbiome interactions. That means your gut microbes, your intestinal nerves, your spinal cord, your emotional centers in the brain, and your stress hormones are all talking to each other… and something’s gone wrong in the conversation.
The Gut-Brain Axis: Your Body’s Hidden Wiring System
Think of your gut as a second brain. It has its own nervous system-the enteric nervous system-with over 100 million neurons. These neurons are wired directly to your central nervous system via the vagus nerve, the longest cranial nerve in your body. This is the gut-brain axis: a two-way highway.
When you’re stressed, your brain sends signals down that highway telling your gut to slow down or speed up. But in IBS, the reverse also happens. Your gut sends up distress signals-because of bloating, gas, or irritated nerves-and your brain interprets them as pain, even when there’s no damage. Brain scans show this clearly: people with IBS have thicker gray matter in areas that process pain and emotion, and thinner gray matter in areas that help control those feelings.
And it’s not just nerves. Your gut makes 95% of your body’s serotonin-a neurotransmitter that affects mood, sleep, and bowel movement. In IBS-D (diarrhea-predominant), serotonin levels in the gut are 60% higher than normal. In IBS-C (constipation-predominant), they’re too low. That’s why drugs targeting serotonin receptors can help. But it’s not just serotonin. Dopamine, GABA, histamine, and even your immune cells are involved. Studies show IBS patients have lower levels of β-endorphin, your body’s natural painkiller, right where it’s needed-in the colon.
Why Your Gut Microbes Matter More Than You Think
Your gut is home to trillions of bacteria. In a healthy person, Firmicutes and Bacteroidetes-the two main types-live in balance. In IBS, that balance is off. This isn’t just about bad bacteria. It’s about what they produce. When certain microbes ferment food too quickly, they release gas, draw water into the intestine, and trigger bloating and cramps. That’s why the low-FODMAP diet works for 50-76% of people. FODMAPs are short-chain carbs that feed these microbes. Cutting them back reduces the fermentation firestorm.
But it’s not just diet. Your microbes also influence your brain. They produce chemicals that cross into your bloodstream and affect your mood and pain sensitivity. One probiotic strain, Bifidobacterium infantis 35624, has been shown in clinical trials to reduce bloating and pain in 30-40% of IBS patients-twice as well as placebo. Fecal microbiota transplants (FMT) have shown promise too, but results vary wildly depending on the donor. It’s not magic. It’s microbiome repair.

Why Traditional Medications Often Fail
Antispasmodics, laxatives, and anti-diarrheals like loperamide are still widely prescribed. But they treat symptoms, not the cause. And they come with side effects: dizziness, dry mouth, constipation, even heart rhythm issues. A Reddit survey of 142,000 IBS patients found that 63% had to stop traditional meds because of side effects. Forty-seven percent quit within three months.
Even newer drugs have limits. Alosetron, a serotonin blocker for IBS-D, helps about half of women-but carries a rare but serious risk of ischemic colitis. Prucalopride, for IBS-C, improves constipation in about half of users. But neither fixes the brain-gut miscommunication. That’s why many people feel like they’re stuck in a cycle: take the pill, feel better for a week, then symptoms creep back.
What Actually Works: Evidence-Based Relief Strategies
There are three proven approaches that target the gut-brain axis directly-and they work better than pills.
1. Low-FODMAP Diet (with guidance)
This isn’t just cutting out onions and garlic. It’s a three-phase process: elimination, reintroduction, and personalization. Done right-with a dietitian-it helps 50-76% of people. But 65% find the first phase (4-6 weeks of strict restriction) too hard. That’s why working with a specialist matters. You’re not eliminating forever. You’re finding your triggers.
2. Gut-Directed Hypnotherapy
This isn’t stage hypnosis. It’s a structured therapy where you learn to calm your gut-brain signals. In randomized trials, 70-80% of people report major symptom improvement-double the rate of standard care. And the effects last. A 2021 study showed benefits still there six months later. The catch? It’s hard to find. There’s only about one certified practitioner per 500,000 people in rural areas. Sessions cost $1,200-$2,500 out of pocket. But for many, it’s life-changing.
3. Neuromodulation: tVNS and Beyond
Transcutaneous vagus nerve stimulation (tVNS) is a new, non-invasive option. You wear a small device behind your ear that sends gentle pulses to the vagus nerve. Pilot studies show 45-55% reduction in abdominal pain. Larger trials are underway. It’s not FDA-approved for IBS yet, but it’s available in clinics in Australia, the U.S., and Europe. Some people use it alongside hypnotherapy for stronger results.
What No One Tells You About Getting Diagnosed
Most people wait 3-7 years to get diagnosed. Forty-two percent see five or more doctors. Why? Because IBS is a diagnosis of exclusion. Your doctor rules out celiac, Crohn’s, cancer, and infections first. But many doctors still don’t know the latest brain-gut science. They don’t ask about stress, sleep, or mood. They don’t explain serotonin or the vagus nerve. That leaves patients feeling dismissed.
Here’s what helps: if your doctor explains the gut-brain axis to you, you’re 30% more likely to stick with treatment and 25% more likely to see improvement. Knowledge is power. That’s why resources like the Mayo Clinic’s Gut-Brain Axis Toolkit score 4.7/5 among clinicians. Most patient websites? They’re oversimplified. Don’t trust them.

The Future: Personalized Medicine for IBS
By 2026, things are changing fast. In 2023, the first gut-brain biomarker panel, VisceralSense™, launched. It measures 12 microbial metabolites and neurotransmitter ratios to predict which treatment will work for you-with 85% accuracy. No more guessing. No more trial and error.
Pharmaceutical companies are pouring money into this. A new drug called etrasimod, tested in 2023, improved symptoms in 52% of IBS-D patients versus 31% on placebo. The NIH has launched a $15 million project to build personalized treatment algorithms based on your unique gut-brain profile. The European Gut-Brain Atlas Project is mapping every neural connection between gut and brain by 2027.
This isn’t science fiction. It’s happening now. The IBS market is projected to hit $4.1 billion by 2027, with gut-brain therapies growing at 15% a year. In five years, the old model-pills for diarrhea or constipation-will be outdated. The future is precision: matching your biology to your treatment.
Where to Start Today
If you have IBS, here’s what to do next:
- Find a doctor who knows about the gut-brain axis. Ask: "Do you treat IBS as a brain-gut disorder?" If they say no, find someone else.
- Try the low-FODMAP diet-but work with a registered dietitian. Don’t do it alone.
- Look for gut-directed hypnotherapy. Search for certified practitioners through the American Society of Clinical Hypnosis or the British Society of Gastroenterology.
- Consider tVNS if you’re in Australia, the U.S., or Europe. Some clinics offer trial sessions.
- Track your symptoms. Use a simple app or notebook: note food, stress, sleep, bowel movements. Patterns will emerge.
IBS isn’t your fault. It’s not weakness. It’s a complex, biological system out of sync. But it’s not untreatable. The tools to fix it exist. They’re just not in your doctor’s office yet. You have to seek them out. And you can.
Is IBS just stress or anxiety?
No. While stress can make IBS worse, it doesn’t cause it. IBS is a real physical disorder involving miscommunication between your gut and brain. Brain scans show structural changes in IBS patients, and their gut produces abnormal levels of serotonin and other chemicals. Anxiety and depression are common because the nervous system is overactive-not because the symptoms are "all in your head." Treating mental health helps, but it doesn’t cure IBS alone.
Can probiotics help with IBS?
Yes-but only specific strains. Bifidobacterium infantis 35624 is the most studied and proven to reduce bloating and pain in clinical trials. Other strains like Lactobacillus plantarum 299v and Saccharomyces boulardii also show benefit. Most store-bought probiotics won’t help. Look for products with these exact strains and doses (at least 1 billion CFUs). Avoid multi-strain blends unless they include these proven ones.
Why does the low-FODMAP diet work?
FODMAPs are short-chain carbs that are poorly absorbed in the small intestine. In IBS, they draw water into the gut and get rapidly fermented by gut bacteria, producing gas and stretching the intestinal wall. This triggers pain signals in people with a hypersensitive gut. The low-FODMAP diet reduces this fermentation and distension. It’s not about eliminating carbs forever-it’s about identifying your personal triggers through a structured reintroduction phase.
Is IBS curable?
There’s no cure yet, but many people achieve long-term remission. Studies show that with the right combination of diet, gut-directed hypnotherapy, and lifestyle changes, up to 70% of people can reduce symptoms by 70% or more. The goal isn’t perfection-it’s control. You can live without constant pain, bloating, or bathroom emergencies. It takes time and the right tools, but it’s possible.
What’s the difference between IBS and IBD?
IBS (Irritable Bowel Syndrome) is a functional disorder-no inflammation or damage to the gut lining. IBD (Inflammatory Bowel Disease), which includes Crohn’s and ulcerative colitis, involves actual inflammation, ulcers, and tissue damage visible on scans and biopsies. IBS doesn’t increase cancer risk. IBD does. Blood tests and colonoscopies can tell them apart. Many people with IBS are wrongly told they have IBD-or vice versa-so accurate diagnosis matters.
Can IBS symptoms change over time?
Yes. Many people switch between IBS-D (diarrhea), IBS-C (constipation), and mixed types over months or years. Hormones, stress, diet, and gut microbiome shifts all play a role. A woman might have more diarrhea during her period. Someone might develop constipation after antibiotics. This variability is normal. It doesn’t mean you’re getting worse-it means your gut-brain axis is sensitive to change. Tracking patterns helps you adapt your treatment.
Are there any new treatments coming soon?
Yes. Etrasimod, a new oral drug targeting immune signaling in the gut, showed 52% symptom improvement in phase III trials in late 2023. A second-generation FMT product with standardized microbial strains is expected by 2026. Wearable tVNS devices are being approved for home use. And by 2027, personalized treatment plans based on your gut microbiome and brain activity will become available in major clinics. The next five years will transform how IBS is treated.
What to Do If You’re Feeling Overwhelmed
IBS is exhausting. You’re not lazy. You’re not broken. You’re navigating a complex, invisible condition in a healthcare system that still treats it like a minor inconvenience. But you’re not alone. The science is finally catching up. The tools are getting better. And the more you understand your gut-brain axis, the more power you have.
Start small. One change. One conversation with a doctor. One session with a dietitian. One day without FODMAPs. Progress isn’t linear. But it’s real. And it’s within reach.




Mohammed Rizvi
January 25, 2026 AT 20:13