pricepropharmacy.com Review: Safe, Affordable Online Pharmacy & Prescription Drug Savings
July 2 2025Antibiotic therapy: smart use, resistance, and practical tips
Up to 30% of outpatient antibiotic prescriptions are unnecessary. That matters because unnecessary use fuels resistance and raises your risk of side effects. This short guide gives clear, practical steps to use antibiotics safely, how to spot problems early, and what to ask your clinician when antibiotics are on the table.
Start by asking why you need one. Is it bacterial or viral? Antibiotics don't touch viruses like colds or most sore throats. If your doctor prescribes antibiotics, ask which bacteria they target, how long to take the drug, and whether you need tests or follow-up. Knowing the reason makes it easier to stick with the plan.
Take it right — dosing, duration, and missed doses
Take antibiotics exactly as prescribed. Skipping doses or stopping early can let bacteria survive and develop resistance. If you miss a dose, take it as soon as you remember unless the next dose is near; never double up. The prescribed duration matters — shorter can be OK for some infections, longer for others. Ask whether a shorter course is safe for your situation.
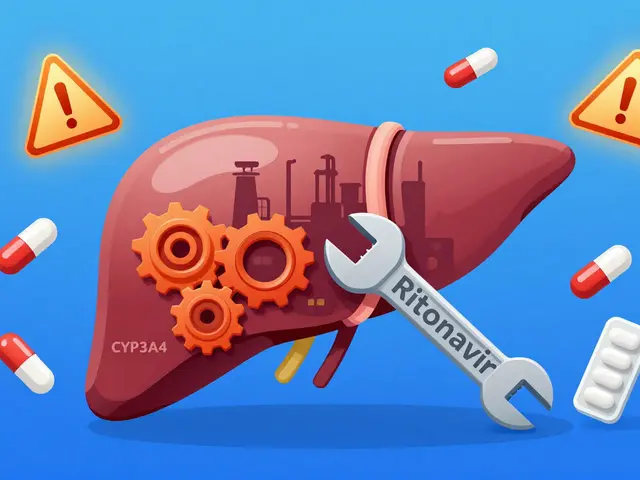
Pay attention to interactions. Common meds like antacids, blood thinners, and some antidepressants can change antibiotic levels. Tell your provider about all medicines, supplements, and herbal products you use. Also mention allergies — if you had a rash or breathing trouble from an antibiotic before, remind your prescriber.
Side effects, probiotics, and what to watch for
Stomach upset, diarrhea, and yeast infections are common. Most side effects are mild and pass quickly, but severe reactions like high fever, rash, swelling, or breathing trouble need emergency care. If you develop severe diarrhea, especially with belly pain or blood in the stool, call your doctor — that could be C. difficile, which needs prompt treatment.
Want to reduce gut upset? Taking a probiotic like Lactobacillus or eating yogurt with live cultures can help, but don't use probiotics instead of medical advice. Also avoid alcohol with certain antibiotics — ask if yours has a warning.
Finish the course unless told otherwise, and return if symptoms worsen or don't improve in 48–72 hours. Keep unused pills out of reach and dispose of them safely — don't share antibiotics or keep leftover pills for later.
Traveling? Carry a copy of your prescription, check rules for bringing medicines through borders, and store drugs as advised. If you’re being treated for an infection that spreads easily, follow hygiene tips to avoid passing it on.
If your infection doesn't clear or comes back, ask for a culture and sensitivity test. That tells which antibiotic will work best. Avoid pushing for broad-spectrum drugs when a targeted antibiotic will do — targeted therapy reduces side effects and slows resistance. Keep records of treatments to help future care and recovery.
Finally, antibiotic stewardship is partly on you. Ask questions, follow instructions, and avoid pressuring clinicians for antibiotics when they're not needed. Smart use protects your health now and keeps antibiotics working for the future.
 5 May
5 May
Ampicillin for the Treatment of Brucellosis: A Comprehensive Guide
As a blogger, I wanted to share my comprehensive guide on using Ampicillin for the treatment of Brucellosis. Ampicillin is an antibiotic that has proven to be effective in combating this bacterial infection, which affects both humans and animals. In my guide, I discuss the proper dosage and duration of treatment, as well as potential side effects and precautions to consider. I also explore alternative treatment options for those who may be allergic to Ampicillin or unable to take it for other reasons. Overall, I hope this guide serves as a valuable resource for anyone affected by Brucellosis and seeking information on Ampicillin as a treatment option.
Read More...