Buy-Pharma-MD: Your Guide to Safe and Affordable Online Pharmacy Shopping
July 29 2025Ammonia Reduction: What It Is and Why It Matters
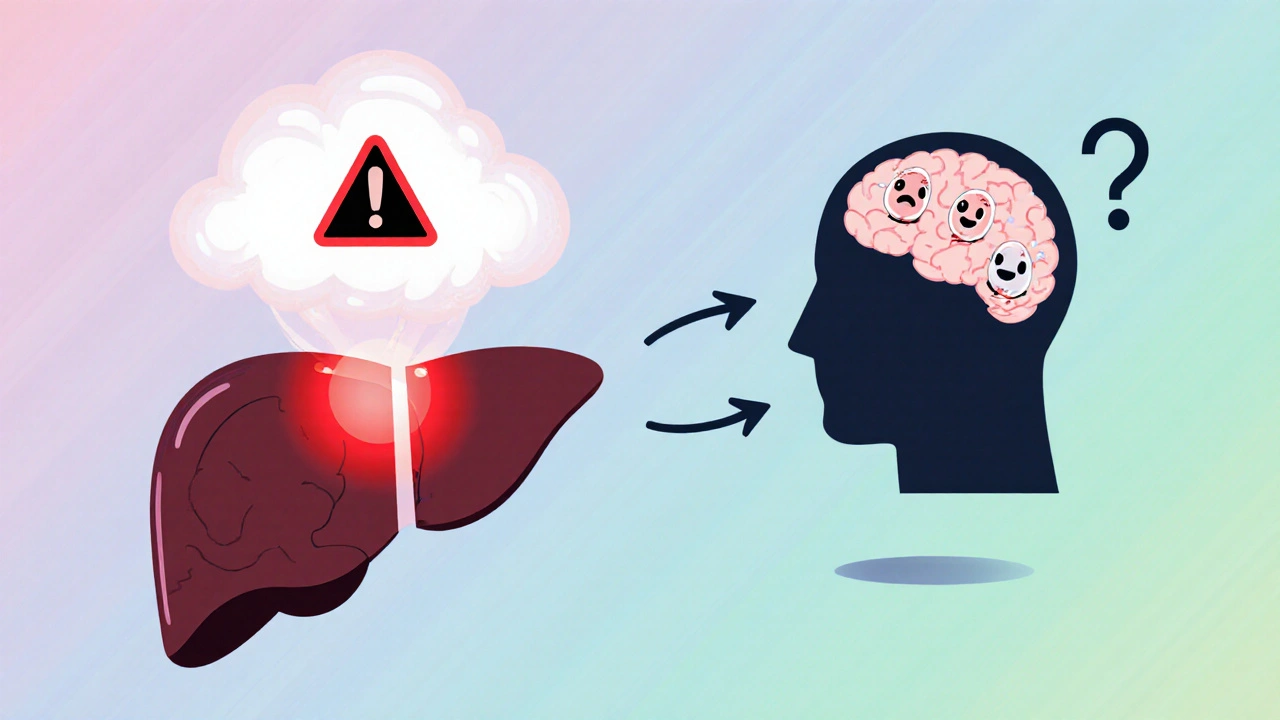
When working with ammonia reduction, the process of lowering excess ammonia in the bloodstream. Also known as blood ammonia control, it helps prevent neurological symptoms and supports overall liver health.
The body turns protein‑derived nitrogen into urea through the urea cycle, a series of liver‑based reactions that convert toxic ammonia into safe, excretable waste. When the cycle stalls—because of liver disease, certain medications, or high protein intake—ammonia builds up, leading to confusion, fatigue, or worse. Understanding how liver function and kidney clearance interact with the urea cycle is the first step toward effective ammonia reduction.
Key Factors That Influence Blood Ammonia
Three main players drive ammonia levels: dietary protein, the amount and type of protein you eat, liver health, how well your liver can run the urea cycle, and kidney function, the kidneys' ability to filter and excrete urea. Each factor creates a semantic triple: *Ammonia reduction* requires *dietary protein adjustment*; *Liver health* influences *blood ammonia*; *Kidney function* supports *urea elimination*.
First, look at protein. Not all proteins raise ammonia equally. Plant‑based sources like lentils and tofu tend to produce less ammonia than red meat because they contain more non‑essential amino acids that the liver can recycle. A simple rule is to keep total protein around 0.8 g per kilogram of body weight unless your doctor says otherwise. Spreading protein across meals also helps the urea cycle keep pace.
Second, protect your liver. If you have cirrhosis or hepatitis, avoiding alcohol, limiting high‑fructose foods, and staying on prescribed liver‑support supplements (such as L‑ornithine‑L‑aspartate) can keep the urea cycle humming. Research shows that L‑ornithine‑L‑aspartate reduces blood ammonia by up to 30 % in chronic liver disease patients.
Third, watch the kidneys. Dehydration reduces urine output, slowing urea clearance. Aim for at least 2 liters of water daily, and consider a modest amount of potassium‑rich foods (bananas, oranges) to help renal excretion. If you’re on diuretics, talk to your doctor about adjusting the dose.
Medications also play a role. Some antibiotics (e.g., rifaximin) and lactulose are prescribed specifically to trap ammonia in the gut and prevent absorption. Even over‑the‑counter antacids can affect gut flora, indirectly influencing ammonia production.
Finally, lifestyle tweaks matter. Regular light exercise boosts circulation, helping the liver and kidneys clear toxins faster. Stress management—through meditation or simple breathing exercises—can lower cortisol, which otherwise raises protein catabolism and ammonia generation.
Putting all these pieces together, you can craft a personal plan for ammonia reduction. Start with a protein audit, add liver‑friendly foods, stay hydrated, and discuss any needed meds with your clinician. Below, you’ll find articles that dive deeper into each of these strategies, from diet hacks to medication comparisons, giving you actionable steps to keep your blood ammonia in check.
 20 Oct
20 Oct
Probiotics for Hepatic Encephalopathy: Treatment Insights
Learn how probiotics can aid hepatic encephalopathy treatment, from the science behind gut‑liver interaction to practical tips and clinical evidence for patients and caregivers.
Read More...




