When you're taking lithium for bipolar disorder, even small changes in your body or medications can have big consequences. Lithium isn't like most drugs. It works in a very narrow range - too little and it doesn't help; too much and it can land you in the hospital. The difference between a safe dose and a dangerous one is razor-thin. That’s why lithium interactions with common over-the-counter meds, diuretics, and even how much water you drink matter more than you think.
How Lithium Works - and Why It’s So Fragile
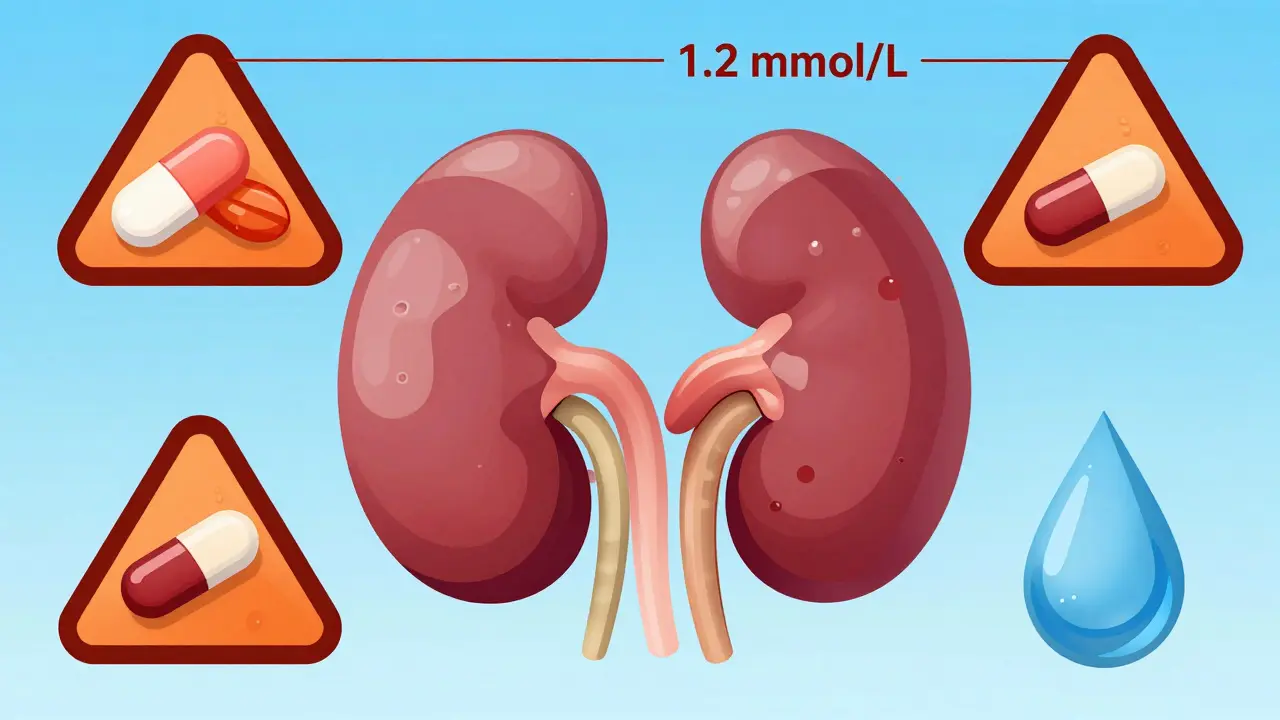
Lithium is cleared from your body almost entirely by your kidneys. About 95% of it leaves your system unchanged through urine. That means anything that affects kidney function - whether it’s a drug, dehydration, or an illness - can cause lithium to build up. Your kidneys don’t just filter waste. They also fine-tune how much lithium gets reabsorbed. When that balance shifts, lithium levels spike. And once they go above 1.2 mmol/L, you’re in danger zone.
Older adults are especially at risk. People over 65 are more than three times as likely to experience lithium toxicity. Why? Kidney function naturally declines with age. Combine that with other health issues like heart failure or high blood pressure, and you’ve got a perfect storm. Even healthy-looking people can be at risk if they’re on multiple medications or don’t drink enough water.
NSAIDs: The Silent Lithium Boosters
NSAIDs - things like ibuprofen, naproxen, and diclofenac - are common pain relievers. You might grab them for a headache, sore back, or arthritis. But if you’re on lithium, these drugs can quietly push your lithium levels into the toxic range. How? They block prostaglandins in your kidneys. These are natural chemicals that help keep blood flow steady in the kidneys. When prostaglandins drop, kidney filtration slows. Lithium doesn’t get flushed out. It piles up.
The numbers don’t lie. Studies show NSAIDs can reduce lithium clearance by 25% to 50%. Indomethacin is the worst offender - it can spike lithium levels by 30% to 60%. Even ibuprofen, which many people think is safe, can raise levels by 25% to 40%. Celecoxib is a bit better, but still carries a 15% to 30% risk. The interaction hits fast - often within the first week of taking the NSAID. And it doesn’t matter if you only take it occasionally. Regular use is worse, but even one or two doses can be enough to tip someone over the edge.
There’s a scary case from New Zealand: a 72-year-old woman on lithium and an ACE inhibitor for high blood pressure. She started taking an NSAID for joint pain. Her lithium levels weren’t checked for weeks. Within days, she developed severe toxicity and died. That’s not rare. It’s preventable.
Diuretics: The Big Culprits
Diuretics - or water pills - are meant to help your body get rid of extra fluid. But with lithium, they do the opposite. They make lithium stick around longer.
Thiazide diuretics like hydrochlorothiazide are the most dangerous. They can raise lithium levels by 25% to 50% within just 7 to 10 days. Why? They change how your kidneys handle sodium. Lithium and sodium are handled by the same transport system. When thiazides reduce sodium reabsorption, your kidneys start reabsorbing more lithium instead. It’s a sneaky swap.
Loop diuretics like furosemide (frusemide) are less risky, but still dangerous. They can bump lithium up by 10% to 25%. And potassium-sparing diuretics like spironolactone? The data is mixed. Some studies show a small rise, others show no effect. But here’s the twist: osmotic diuretics like mannitol and carbonic anhydrase inhibitors like acetazolamide actually lower lithium levels by 15% to 30%. That’s right - some diuretics can make lithium less effective, which is its own kind of risk.
And don’t forget herbal diuretics. Many weight-loss teas and supplements claim to be “natural” and “safe.” But if they contain ingredients like dandelion, parsley, or green tea extract, they can act like diuretics. And they’re not monitored. One woman in Australia ended up in the ER after taking a “detox” tea for a week. Her lithium level jumped 22%.
Dehydration: The Invisible Threat
You don’t need to be sick to be at risk. Just skipping a few drinks, sweating through a workout, or flying across the country can be enough. Lithium levels rise when your body loses water - even mild dehydration. Losing just 2% to 3% of your body weight in fluid can increase lithium concentrations by 15% to 25%. That’s like taking a dose of NSAIDs without even realizing it.
Sodium plays a big role too. If you suddenly cut back on salt - maybe you’re trying a low-sodium diet - lithium levels climb. Eating more salt lowers them. It’s not about being unhealthy. It’s about consistency. A sudden drop in sodium intake of 20 to 30 mmol/day can shift lithium levels by 10% to 20%. That’s enough to trigger symptoms.
Travelers are especially vulnerable. Flying long-haul, hiking in hot weather, or getting sick with vomiting or diarrhea all lead to fluid loss. That’s why experts say: if you’re on lithium, carry water everywhere. Drink even if you’re not thirsty. And if you’re sick, check your lithium level before and after.
Symptoms You Can’t Ignore
Lithium toxicity doesn’t always come with a siren. Early signs are subtle - and easily mistaken for something else. Diarrhea? That’s the most common early warning. About 68% of people with early toxicity report it. Then come lightheadedness (52%), drowsiness (47%), and tremors. You might think it’s just a bug or fatigue. But if you’re on lithium, it’s a red flag.
As levels climb, you might notice blurred vision (31%), ringing in the ears (29%), or confusion. At severe levels, seizures, kidney damage, or coma can happen. And here’s the worst part: some kidney damage from lithium toxicity is permanent. Especially in older people or those with pre-existing kidney problems.

What to Do - And What to Avoid
Here’s the bottom line: lithium interactions are not theoretical. They kill. But they’re also preventable.
- Avoid NSAIDs if you can. Use acetaminophen (paracetamol) instead for pain. It doesn’t affect lithium.
- Never start a new diuretic without talking to your doctor. Thiazides are especially risky. If you need one, your lithium dose may need to be cut by 25% to 50%.
- Hydrate. Drink water every day. Even if you’re not thirsty. Especially in heat, after exercise, or when you’re sick.
- Don’t change your salt intake suddenly. Keep it steady. No crash diets or extreme low-salt plans.
- Get your lithium levels checked within a week of starting any new medication. And again after two weeks. Then monthly for the first few months.
- Tell every doctor you see - even your dentist - that you’re on lithium. Many don’t ask.
If you feel off - dizzy, nauseous, shaky - don’t wait. Get your lithium level checked. It takes 15 minutes. It could save your life.
Monitoring Is Non-Negotiable
Clinical guidelines are clear: if you’re on lithium and start an NSAID or diuretic, check your levels weekly for at least a month. Then continue regular checks. Your doctor should also monitor your kidney function - creatinine and eGFR - every 3 to 6 months. And if you’re over 65, have heart disease, or take multiple meds, you should be under shared care with a nephrologist or specialist.
Electronic health systems now flag these interactions. But as the New Zealand case shows, alerts aren’t enough. People still get missed. You have to be your own advocate. Keep a log of your meds. Note when you start or stop anything. Write down how much water you drink. If something feels wrong, speak up.
Can I take ibuprofen if I’m on lithium?
It’s risky. Ibuprofen can raise lithium levels by 25% to 40%. If you must take it, use the lowest dose for the shortest time. Always check your lithium level before and after. Better yet, switch to acetaminophen (paracetamol), which doesn’t interact with lithium.
What if I accidentally take an NSAID?
Don’t panic, but act fast. Stop the NSAID. Drink plenty of water. Contact your doctor immediately. They’ll likely order a lithium level test within 24 to 48 hours. If your level is rising, they may hold your next lithium dose and monitor you closely.
Are all diuretics dangerous with lithium?
No, but most are. Thiazide diuretics like hydrochlorothiazide are the most dangerous, raising lithium by 25% to 50%. Loop diuretics like furosemide are less risky but still require monitoring. Osmotic diuretics like mannitol and acetazolamide actually lower lithium levels, so they’re used differently. Always check with your doctor before starting any new diuretic.
How much water should I drink daily if I’m on lithium?
Aim for 2 to 3 liters per day - more if you’re active, in heat, or sick. Don’t wait until you’re thirsty. Drink regularly. If you’re traveling, flying, or sweating a lot, increase your intake. Dehydration as small as 2% body weight loss can raise lithium levels by 15% to 25%.
Can changing my diet affect lithium levels?
Yes. Sodium intake directly affects lithium. Eating less salt increases lithium levels. Eating more lowers them. A change of 20 to 30 mmol/day in sodium (roughly 1 to 1.5 teaspoons of salt) can shift lithium levels by 10% to 20%. Keep your salt intake steady. Don’t suddenly go on a low-sodium diet without talking to your doctor.
What should I do if I get sick with vomiting or diarrhea?
Stop taking lithium until you’re back to normal - but only if your doctor says so. Drink fluids with electrolytes (like oral rehydration solutions). Contact your prescriber immediately. Lithium levels can spike dangerously during illness. You may need a blood test within 24 hours.
Final Thought: Stay in Control
Lithium works. It saves lives. But it demands respect. You can’t treat it like any other medication. It’s not about being careful - it’s about being consistent. Drink water. Know your meds. Talk to your doctor. Track your symptoms. If you’re on lithium, you’re not just taking a pill. You’re managing a delicate balance. And that balance depends on you.






Charlotte Dacre
February 16, 2026 AT 06:19