Many mothers worry that taking medication while breastfeeding will harm their baby. The truth is, 98% of medications are safe to use during breastfeeding when timed correctly. You don’t have to choose between your health and your baby’s. With the right strategy, you can keep nursing while managing pain, depression, anxiety, or other conditions - without putting your infant at risk.
Why Timing Matters More Than You Think
Medication doesn’t flood into breast milk all at once. It follows a predictable pattern based on how your body processes it. Drugs enter your bloodstream, then pass into breast milk mostly when your blood levels are highest. That’s called the peak plasma concentration. After that, your body starts clearing the drug, and milk levels drop. If you take a pill right before feeding, your baby gets the highest dose. But if you time it right - right after a feeding, or before the longest stretch of sleep - your baby gets far less. Think of it like pouring water into a cup. If you pour while your baby is drinking, they get the full glass. But if you pour after they’ve finished, and wait until the next time they’re hungry, they get mostly clean water.How to Time Doses: The Simple Rules
There are two main approaches, depending on how often you need to take your medication.- For once-daily doses: Take your medication right after your baby’s longest sleep period - usually right after bedtime. This gives your body 6 to 8 hours to clear the drug before the next feeding. For example, if your baby sleeps from 10 p.m. to 6 a.m., take your pill at 10:30 p.m. and wait until 6 a.m. to nurse again.
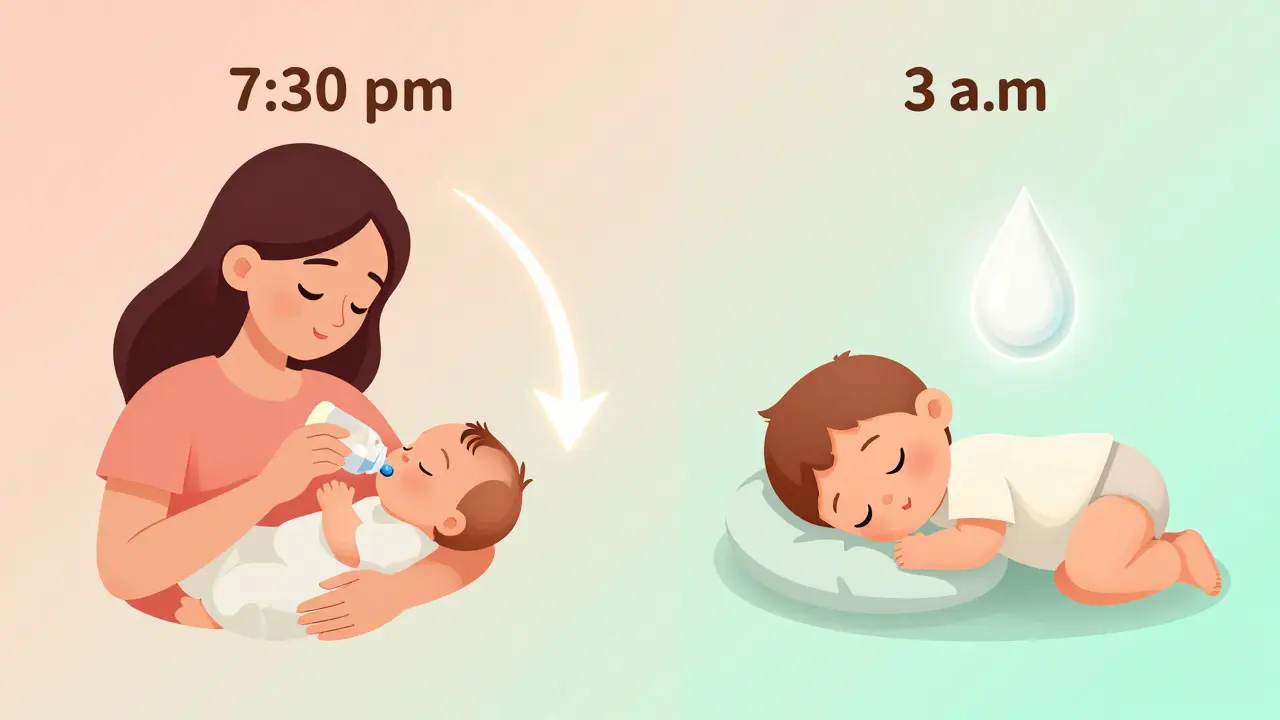
- For multiple daily doses: Breastfeed your baby immediately before taking each dose. This way, the next feeding comes after the drug has had time to clear from your system. If you take a pill at 8 a.m., 2 p.m., and 8 p.m., nurse at 7:30 a.m., 1:30 p.m., and 7:30 p.m.
Which Medications Need the Most Care?
Not all drugs behave the same. Some clear quickly. Others stick around for days. Short-acting drugs (best for timing):- Hydrocodone - peaks in 30 minutes to 2 hours, half-life of 3-4 hours. Nurse right before dosing. Safe at doses under 30 mg daily.
- Oxycodone - peaks in 30 minutes to 2 hours, half-life 3-4 hours. Same timing rules apply.
- Lorazepam - peaks in 1-2 hours, half-life 10-20 hours. Lower transfer to milk than other benzodiazepines. Preferred over diazepam.
- Paroxetine and sertraline - SSRIs with half-lives under 30 hours. Safe and effective when timed properly. Avoid fluoxetine - its active metabolite stays in your system for over 10 days.
- Diazepam - peaks in 30 minutes to 2.5 hours, but half-life is 44-48 hours. It builds up over time. Even with timing, some babies may get sleepy or have trouble feeding. Use only if no better option exists.
- Extended-release alprazolam - peaks at 9 hours. Hard to time. Stick with immediate-release if possible.
- Prednisone - at standard doses, almost no transfer. But if you’re on a high dose (over 20 mg), wait 4 hours after taking it before nursing.
Special Cases: Newborns, Premies, and Sick Babies
Not all babies are the same. Newborns, especially those born early or with health problems, process drugs much slower than older infants. Their livers and kidneys aren’t fully developed.- For babies under 2 weeks old, even safe medications can build up. Be extra careful with timing.
- For premature babies or those with kidney or liver issues, avoid long-acting drugs entirely if possible.
- Watch for signs your baby might be affected: unusual sleepiness, poor feeding, irritability, or slow weight gain.
What About Pumping and Dumping?
Some moms think they need to pump and throw away milk after taking medication. That’s rarely necessary - and it can hurt your supply. There’s one exception: if you’re taking a short-term medication like a strong painkiller after surgery, and you’re worried about a single exposure. In that case, pump and store milk before your dose. Use that stored milk for the next 4-6 hours after taking the drug. One mother in Cambridge shared her experience: “I pumped 8 ounces before my dental surgery with hydrocodone. Fed that to my 6-month-old for the next 4 hours. No issues.” That’s smart planning - not fear-driven dumping. Don’t pump and dump unless your doctor says so. It won’t make you safer - it might just make you exhausted.Tools to Help You Get It Right
You don’t have to remember half-lives or peak times. There are reliable, free resources built for this exact purpose.- LactMed - a database from the National Library of Medicine. Updated monthly. Search any medication and get clear timing advice, RID percentages, and safety ratings.
- Hale’s Medication and Mothers’ Milk - the gold standard reference. Uses a 5-level safety scale. Look for L1 or L2 ratings - those are safest.
- LactMed app - free on iOS and Android. Over 127,000 users. Works offline. Great for quick checks at 2 a.m.
When to Talk to a Specialist
Most primary care doctors and even some OB-GYNs aren’t trained in breastfeeding pharmacology. A 2021 study found only 58% could correctly time common medications. If you’re taking:- Psychiatric meds (SSRIs, benzodiazepines)
- Opioids or painkillers
- Chronic condition drugs (thyroid, epilepsy, high blood pressure)
- Any drug with a half-life over 24 hours

What to Avoid
Some drugs should be avoided altogether while breastfeeding:- Fluoxetine - too long half-life (96 hours). Can cause jitteriness or poor feeding in babies.
- Chloramphenicol - can cause gray baby syndrome.
- Lithium - accumulates in milk. Requires strict monitoring.
- Radioactive isotopes - used in scans. You’ll need to stop nursing temporarily.
Real Success Stories
A 2023 study from the Women’s Mental Health Specialty Clinic followed 125 mothers taking SSRIs. 92% continued breastfeeding successfully by timing doses right before feedings. No babies showed signs of sedation or withdrawal. Another mom in London took hydrocodone after a C-section. She nursed at 7 p.m., took her pill at 8 p.m., and didn’t nurse again until 3 a.m. Her baby slept through the night - no fussing, no drowsiness. These aren’t rare cases. They’re the rule - when timing is used correctly.Final Tip: Don’t Stress the Perfect Plan
Life with a newborn is messy. Sometimes you’ll forget to time it right. Sometimes your baby wakes up an hour early. That’s okay. The goal isn’t perfection. It’s reduction. Even if you miss the ideal window once, you’re still lowering your baby’s exposure compared to taking the pill right before every feed. And if you’re unsure - ask. Call a lactation consultant. Check LactMed. Talk to your pharmacist. You’re not alone. Thousands of mothers do this every day - safely.Is it safe to take painkillers while breastfeeding?
Yes, most painkillers are safe when timed correctly. Hydrocodone, oxycodone, and ibuprofen are low-risk options. Take them right after feeding, not before. Avoid codeine and tramadol - they can turn into dangerous substances in your baby’s system. Stick to immediate-release forms, not extended-release. Always use the lowest dose needed.
How long should I wait to breastfeed after taking medication?
You don’t need to wait - unless you’re on a long-acting drug like diazepam. For most medications, nurse right before taking your dose. That way, your milk is cleanest when your baby feeds next. If you’re on a once-daily pill, take it after your baby’s longest sleep. No need to wait hours. The goal is to feed when drug levels are lowest, not to delay feeding.
Can I take antidepressants while breastfeeding?
Yes - and it’s often safer than stopping. Sertraline and paroxetine are the most studied and safest options. Fluoxetine should be avoided because it stays in your system for weeks. Timing matters: take your dose right after a feeding. Most babies show no side effects. Untreated depression, however, can harm bonding and infant development - so treating your mental health is part of being a good parent.
Does pumping and dumping help reduce baby’s exposure?
Only in rare cases. Pumping and dumping doesn’t speed up how fast the drug leaves your body - your liver does that. If you pump, you’re just removing milk that already contains the drug. The only time it helps is if you pre-pump before taking a one-time, high-dose medication (like after surgery). Otherwise, it can lower your milk supply and cause unnecessary stress. Don’t pump unless your provider says so.
What if my baby seems sleepy or fussy after I take medication?
Watch for changes: excessive sleepiness, trouble latching, poor weight gain, or unusual irritability. If you notice these, check the drug’s half-life and RID (Relative Infant Dose) on LactMed. If it’s high, talk to your doctor about switching to a safer option. Sometimes a small change - like switching from diazepam to lorazepam - makes a big difference. Never stop medication without medical advice, but do report concerns.







vivek kumar
January 17, 2026 AT 12:31