Drug Interaction Warning Calculator
How Drug Interactions Are Rated
The FDA uses AUC ratio thresholds to determine interaction severity. Contraindicated means serious harm or death could occur. Avoid concomitant use means high risk. Dose adjustment required means you can still use them together with changes.
What this means for patients:
When you open a prescription label or check a drug’s prescribing information, you’re not just reading a list of side effects. You’re looking at a carefully structured system designed to keep patients safe. The FDA drug interaction tables in official labels are one of the most important tools doctors and pharmacists use to avoid dangerous combinations. But they’re not easy to read. If you’ve ever stared at Section 7 and wondered what "AUC ratio ≥1.25" actually means - or why some drugs say "avoid" while others say "use with caution" - you’re not alone.
What the FDA Drug Interaction Table Actually Shows
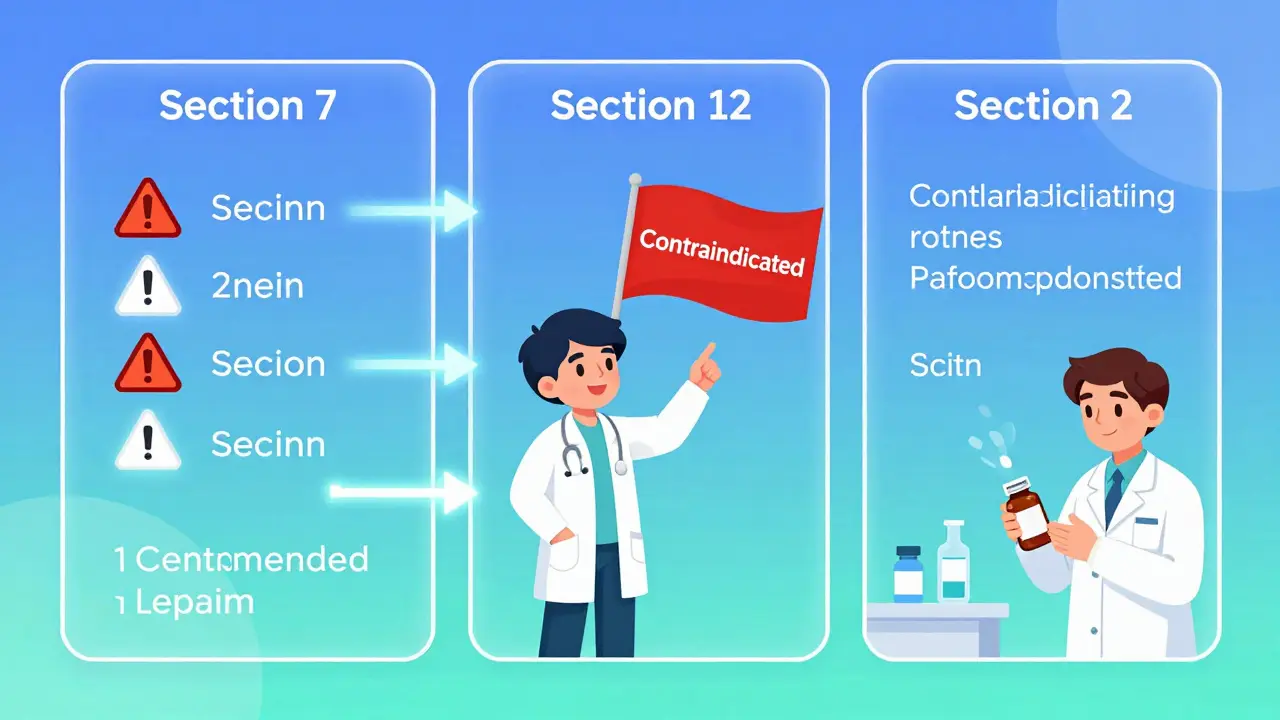
The FDA doesn’t just dump every possible interaction into one long list. It organizes drug interaction data into three clear sections of the prescribing information. Each section serves a different purpose.
Section 7 - Drug Interactions - is where the action is. This is the part you’ll use most. It doesn’t list every lab result or theoretical interaction. It only includes interactions that have been proven to cause real harm in people. According to FDA analysis of 500 drug labels in 2023, this section contains about 85% of the clinical recommendations you need to act on. If a drug says "Contraindicated" with another, it means using them together could cause serious injury or death. "Avoid concomitant use" means the risk is high enough to strongly discourage it. "Dose adjustment required" means you can still use them together - but only if you change the dose.
Section 12 - Clinical Pharmacology - is the science behind Section 7. This is where you’ll find numbers: AUC fold-changes, CYP enzyme inhibition levels, transporter effects. For example, if a drug increases the AUC of another by 2.5-fold, that’s a major change. The FDA now defines a clinically significant interaction as an AUC ratio (AUCR) of 1.25 or higher for CYP enzyme interactions. That means if Drug A raises Drug B’s blood levels by 25% or more, it’s considered risky. For transporter interactions like P-gp, the threshold is even higher - a 1.5-fold increase for drugs like digoxin or edoxaban triggers a warning. This section explains why the warning exists, not just what it says.
Section 2 - Dosage and Administration - gives you the exact steps to take. If a drug interaction requires a dose change, this section tells you how much to lower it, when to monitor levels, and whether to split doses. A 2022 FDA review found that 73% of labels with significant interactions included these precise instructions here. If you’re managing a patient on multiple drugs, this is the section that tells you whether to cut the dose from 10 mg to 5 mg - or to check a blood level before proceeding.
How the FDA Decides What to Include
The FDA doesn’t guess. It uses hard data from clinical studies. Since the August 2024 update of the ICH M12 Guideline, every drug interaction label must be backed by standardized study methods. Researchers now use consistent models to measure how one drug affects another’s absorption, metabolism, or elimination. For example, if a new antidepressant inhibits CYP2D6, they test it against known CYP2D6 substrates like codeine or tamoxifen. They measure the AUC before and after. If the change exceeds 1.25-fold, it gets labeled.
Not all interactions are treated equally. The FDA focuses on drugs with narrow therapeutic windows - where a small change in blood level can mean the difference between effectiveness and toxicity. Warfarin, digoxin, lithium, and some anti-seizure drugs fall into this category. A 20% increase in digoxin levels can cause life-threatening heart rhythms. That’s why even small changes are flagged.
They also look at patient populations. The elderly make up 35% of prescription users, but interaction data often comes from younger, healthier volunteers. A 2022 commentary in Drug Metabolism and Disposition pointed out that older adults metabolize drugs slower, so interactions that seem mild in studies can become dangerous in practice. The FDA is working to fix this gap, but for now, prescribers must adjust for age on their own.

What’s Missing - And Why It Matters
The system works well for common metabolic pathways - especially CYP enzymes like 3A4 and 2D6. But it’s weaker in other areas. About 31% of biologic drugs - like cancer immunotherapies or autoimmune treatments - have little to no interaction data. That’s because they’re not metabolized by liver enzymes. They’re cleared by the immune system, and we don’t yet have reliable tests to predict how other drugs affect that process.
Herbs and supplements are another blind spot. St. John’s Wort, for example, is a known CYP3A4 inducer - it can cut the effectiveness of birth control pills, antidepressants, and even some cancer drugs. But because it’s sold as a supplement, it doesn’t go through the same FDA review. The FDA acknowledges this gap. A 2024 workshop report found that about 20% of serious drug interactions involve herbal products - yet none of them are required to list interactions on their labels.
And then there’s the class problem. The FDA sometimes warns against an entire drug class - say, "calcium channel blockers" - when only a few members of that class actually cause the interaction. A 2023 analysis showed that 42% of labels were inconsistent here. One label might say "avoid amlodipine," while another says "avoid all calcium channel blockers." This creates confusion. A pharmacist might stop a patient’s blood pressure med unnecessarily because the label is vague.
How Doctors and Pharmacists Actually Use It
Most healthcare providers don’t read the whole label from start to finish. They use a three-step shortcut:
- Check Section 7 first - what’s the bottom-line warning?
- Look at Section 2 - what do I need to do? Change the dose? Monitor levels?
- Only if you need to understand why, go to Section 12.
A 2023 study in JAMA Internal Medicine found that hospitals that integrated FDA interaction data directly into their electronic health records (EHRs) cut interaction-related errors by 39%. That’s because the system now auto-alerts when a doctor tries to prescribe a risky combo. But even with alerts, mistakes happen. A 2024 FDA audit found that 28% of providers misinterpreted the difference between "contraindicated" and "dose adjustment required." One nurse thought "dose adjustment" meant "take less often," not "take less amount." That kind of misunderstanding can be deadly.
Pharmacists are often the last line of defense. A Reddit thread from r/Pharmacy in September 2023 showed that 57% of hospital pharmacists had seen cases where the label said "drug class interaction" but didn’t specify which drugs were risky. That left them guessing - and sometimes delaying care while they looked up each drug individually.

What You Can Do to Stay Safe
If you’re a patient, you don’t need to decode AUC ratios. But you can still protect yourself:
- Always tell your doctor and pharmacist about everything you take - including vitamins, herbs, and over-the-counter painkillers.
- Ask: "Is this safe with my other meds?" Don’t assume they’ve checked.
- If you’re on a blood thinner, anti-seizure drug, or cancer treatment, ask if your other meds could affect it.
- Use the FDA’s Drugs@FDA database to look up your prescription. Search by brand or generic name. You’ll see the full prescribing information - including interaction tables.
For prescribers, the key is consistency. Always check Section 7 first. If you’re unsure, go to Section 2. If you’re still confused, look at Section 12. And if the label says "drug class" without specifics - double-check. Ask a pharmacist. Or use a trusted drug interaction checker that pulls from FDA data.
What’s Coming Next
The FDA isn’t done. By 2025, interaction data will be available in machine-readable formats - meaning computers can automatically read and flag risks without human interpretation. A pilot program called "dynamic labeling" is set to launch in Q2 2026. That means if new evidence emerges tomorrow, the interaction warning on your drug’s label could update overnight - no waiting for a new printed package.
The FDA is also working on better ways to label interactions for biologics and older adults. They’re developing new models to predict how cytokines - proteins involved in inflammation - affect drug metabolism. This could change how we treat patients with autoimmune diseases or cancer.
But the biggest change? The system is finally being used the way it was meant to: as a tool for clinical decision-making, not just compliance. The goal isn’t to scare doctors with a long list. It’s to give them the right information, at the right time, in the right way.
What does AUC ratio mean in FDA drug interaction tables?
AUC stands for "area under the curve," which measures how much of a drug is in your bloodstream over time. The AUC ratio compares the level of a drug when taken alone versus when taken with another drug. If the ratio is 1.25 or higher, it means the second drug increased the first drug’s concentration by 25% or more - which the FDA considers clinically significant. For example, if a statin’s AUC increases by 1.5-fold when taken with grapefruit juice, that’s a warning sign.
Why do some drug labels say "avoid" while others say "contraindicated"?
"Contraindicated" means using the two drugs together could cause serious harm or death - it’s a hard stop. "Avoid concomitant use" means the risk is high, but not necessarily life-threatening. You might still use them together if no alternatives exist, but only under close monitoring. The difference matters: one is an absolute rule, the other is a strong recommendation.
Do FDA interaction tables include herbal supplements?
No. Herbal products and dietary supplements are not required to undergo the same FDA review as prescription drugs. While some - like St. John’s Wort or goldenseal - are known to cause dangerous interactions, they rarely appear in official FDA labeling. That’s why it’s critical to tell your doctor about every supplement you take, even if it’s "natural."
Are drug interaction tables the same in other countries?
Most countries now follow the ICH M12 Guideline, so the structure is similar. But the European Medicines Agency (EMA) often includes more detailed quantitative data in its labels, while the FDA focuses on clear clinical actions. Japan has aligned closely with the FDA since 2021. The U.S. system is now used as a model for about 65% of global drug labeling.
Can I trust online drug interaction checkers?
Yes - if they pull data directly from the FDA’s prescribing information. Tools like Lexicomp, Micromedex, and the FDA’s own Drugs@FDA database are reliable. But avoid general websites that list "possible" interactions without citing sources. Many online tools overstate risks or include outdated data. Always cross-check with the official label.



Sarah Barrett
February 13, 2026 AT 17:42