Understanding Heart Failure and Its Impact on Patients
Heart failure is a chronic, progressive condition where the heart is unable to pump blood effectively to meet the body's needs. As a result, patients with heart failure often experience fatigue, shortness of breath, and fluid retention, which can significantly impact their quality of life. In addition, heart failure is a leading cause of hospitalization and mortality worldwide, making it a major public health concern. In this article, we will explore the potential role of rivaroxaban, a novel oral anticoagulant, in the management of heart failure.
Current Treatment Options for Heart Failure
Currently, the mainstay treatment for heart failure includes medications such as angiotensin-converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARBs), beta-blockers, and diuretics. These medications help to reduce the workload on the heart and alleviate symptoms, but they do not directly address the underlying causes of heart failure. Furthermore, many patients continue to experience symptoms and frequent hospitalizations despite optimal medical therapy. This highlights the need for new and innovative treatment options to improve the management of heart failure.
An Overview of Rivaroxaban
Rivaroxaban is a direct oral anticoagulant (DOAC) that specifically targets factor Xa, a key enzyme in the blood clotting process. It has been widely used for the prevention and treatment of venous thromboembolism (VTE) and stroke prevention in patients with non-valvular atrial fibrillation. Rivaroxaban's unique mechanism of action, oral administration, and predictable pharmacokinetics make it an attractive candidate for further investigation in the context of heart failure.
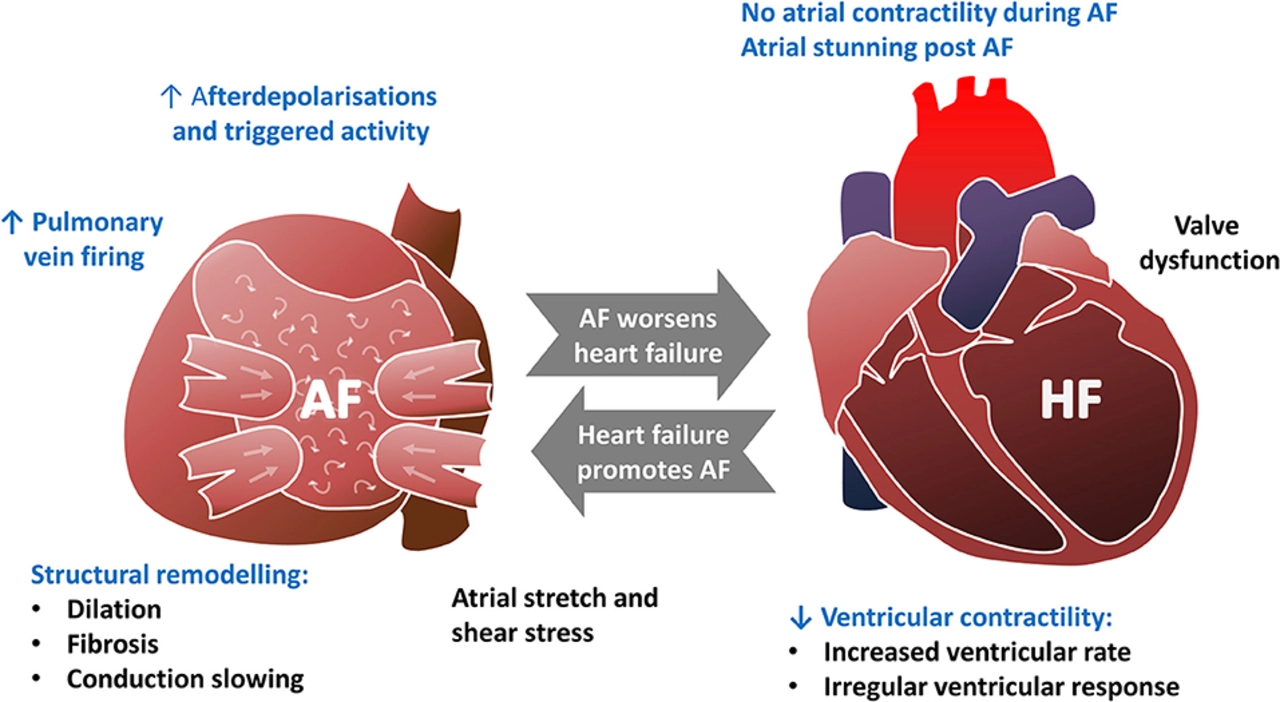
Thrombotic Risk in Heart Failure
Patients with heart failure are at an increased risk of thrombotic events, such as deep vein thrombosis (DVT), pulmonary embolism (PE), and stroke. This is due to several factors, including reduced blood flow, endothelial dysfunction, and increased activation of pro-coagulant factors. Furthermore, heart failure is often associated with atrial fibrillation, which increases the risk of stroke. Therefore, anticoagulant therapy may play a crucial role in preventing thrombotic complications in heart failure patients.
The Potential Role of Rivaroxaban in Reducing Hospitalization and Mortality
Recent clinical trials have investigated the potential benefits of rivaroxaban in patients with heart failure. The COMMANDER HF trial, for example, evaluated the use of rivaroxaban in patients with heart failure and coronary artery disease who were already receiving optimal medical therapy. Although the study did not show a significant reduction in the primary endpoint of all-cause mortality, it did demonstrate a reduction in the rate of hospitalization for heart failure. This finding suggests that rivaroxaban may have a role in reducing the burden of hospitalizations in heart failure patients.
Addressing the Risk of Major Bleeding
One of the main concerns with anticoagulant therapy is the risk of major bleeding complications. In the COMMANDER HF trial, rivaroxaban was associated with a higher risk of major bleeding compared to placebo. However, the risk of intracranial hemorrhage, a particularly concerning type of bleeding, was not significantly increased. It is important for clinicians to carefully weigh the potential benefits of rivaroxaban against the risk of bleeding when considering its use in heart failure patients.
Future Directions in Heart Failure Research
Although the COMMANDER HF trial provided some promising results, further research is needed to better understand the role of rivaroxaban in heart failure management. Future studies should focus on identifying specific patient populations that may benefit most from rivaroxaban therapy, as well as determining the optimal dosing and duration of treatment. Additionally, it will be important to investigate the potential benefits of rivaroxaban in combination with other novel heart failure therapies in order to provide the most comprehensive care for patients.
Conclusion
In conclusion, while the role of rivaroxaban in heart failure management is still under investigation, it presents a promising new avenue for reducing hospitalization and improving patient outcomes. As we continue to learn more about the potential benefits and risks of rivaroxaban in heart failure patients, it is crucial for clinicians and researchers to collaborate in order to optimize patient care and advance our understanding of this complex and challenging disease.




Julien Martin
May 11, 2023 AT 11:09