PSA Screening Isn’t as Simple as It Seems
Every year, millions of men get a simple blood test called PSA to check for prostate cancer. It’s quick, cheap, and often offered as part of a routine checkup. But here’s the thing: getting that test doesn’t always mean you’re getting closer to staying healthy. In fact, for many men, it can lead to more harm than good. The truth is, PSA screening is one of the most debated tools in modern medicine - not because it doesn’t work, but because it works too well at finding cancers that would never hurt you.
What PSA Screening Actually Measures
The PSA test looks for prostate-specific antigen, a protein made by the prostate gland. High levels can signal cancer - but they can also come from a swollen prostate, an infection, even riding a bike. About 75% of men with PSA levels between 4.0 and 10.0 ng/mL end up having a biopsy… and most of them don’t have cancer. That’s not a flaw in the test - it’s how the test works. It’s sensitive, but not specific. And that’s the core of the problem.
Even worse, about 15% of men with aggressive, dangerous prostate cancer have PSA levels below 4.0. That means the test misses some of the worst cases. It’s like using a flashlight to find a hidden door - sometimes it shines right on it, sometimes it misses the mark entirely, and sometimes it just lights up the walls.
The Big Studies That Changed Everything
In the 2000s, two massive studies tried to answer one question: Does PSA screening save lives? The European study (ERSPC) said yes - screening cut prostate cancer deaths by about 21%. But the U.S. study (PLCO) said no - no real difference in death rates. Why the difference? One big reason: in the U.S. study, many men in the "no screening" group ended up getting PSA tests anyway. So the groups weren’t truly different.
What both studies agreed on: screening led to a lot of overdiagnosis. The Cochrane Collaboration found that for every 1,000 men screened over 10 years, 80 to 100 would be diagnosed with prostate cancer that would never cause symptoms. These are cancers that grow so slowly, they’d never be found without screening. But once diagnosed, most men feel they have to do something - surgery, radiation, hormone therapy. And those treatments? They can wreck your quality of life.
The Harms Are Real - and Permanent
Radical prostatectomy, the most common surgery, leads to urinary incontinence in up to 30% of men and erectile dysfunction in 60%. Radiation therapy can cause bowel problems and long-term bladder irritation. And for what? For a cancer that might never have mattered. A 62-year-old man in a 2020 case study had a PSA of 4.7. He had surgery. He lost bladder control. He lost sexual function. His cancer? Low-risk. It would’ve never spread. He was treated for a ghost.
But here’s the flip side: there are men who owe their lives to PSA screening. The Prostate Cancer Foundation’s registry shows 1,247 cases where early detection caught aggressive cancer before it spread. Ninety percent of those men say the test saved their life. So it’s not that screening is useless. It’s that we can’t tell ahead of time who will benefit and who won’t.
Shared Decision-Making: The Only Ethical Way Forward
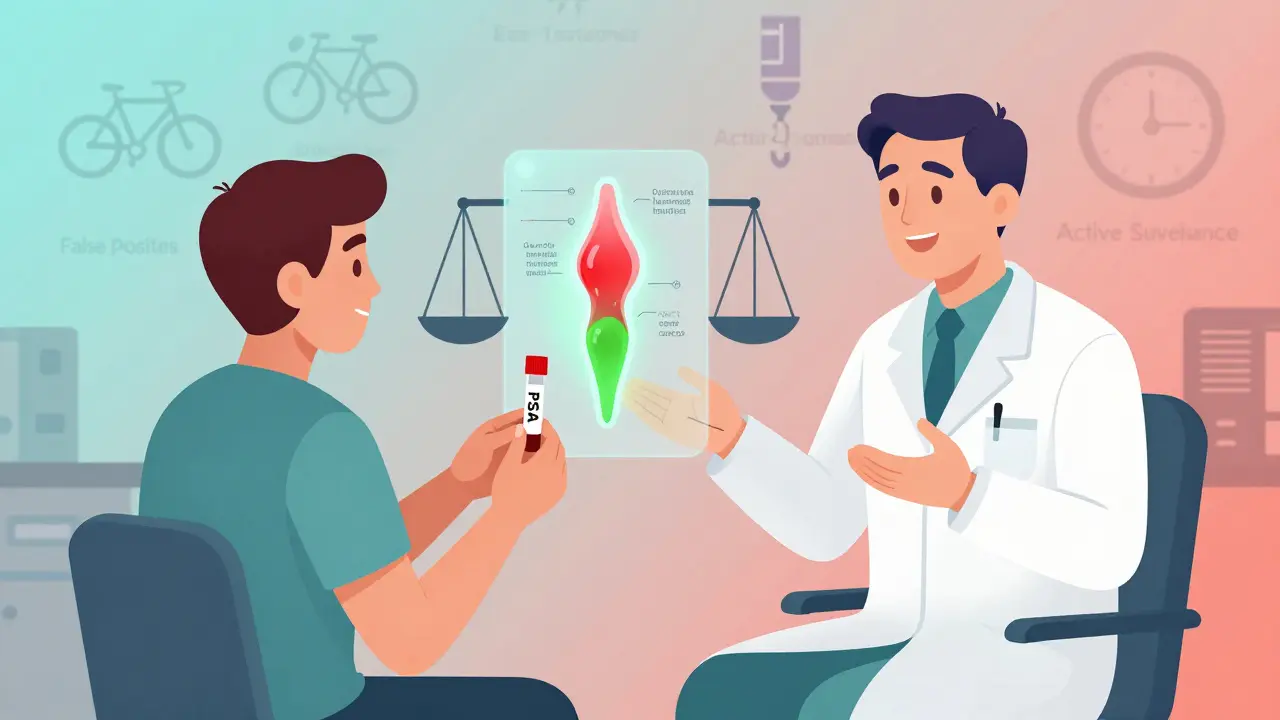
That’s why guidelines from the American Cancer Society, the American Urological Association, and the U.S. Preventive Services Task Force now say the same thing: don’t screen unless you’ve had a real conversation. Shared decision-making means your doctor doesn’t just hand you a test form. They explain: "Here’s what this test can find. Here’s what it can’t. Here’s what happens if we find something. Here’s what happens if we don’t test at all."
It’s not about pushing you one way or the other. It’s about giving you the facts so you can decide what matters to you. Do you want to avoid the risk of side effects, even if it means a small chance of missing a fast-growing cancer? Or are you willing to risk incontinence and impotence to have the best shot at catching something dangerous early?
What Does a Good Conversation Look Like?
Most men say their doctors don’t talk about the downsides. A 2017 survey found only 60% of men who got a PSA test were told about the risks of overdiagnosis or overtreatment. That’s not informed consent - that’s passive consent.
A good discussion takes 15 to 20 minutes. It includes:
- How common prostate cancer is - 1 in 8 men will get it in their lifetime
- How many men die from it - about 35,000 in the U.S. each year
- How many men get treated unnecessarily - 80 to 100 out of every 1,000 screened
- What the side effects of treatment really mean - losing bladder control, losing sexual function
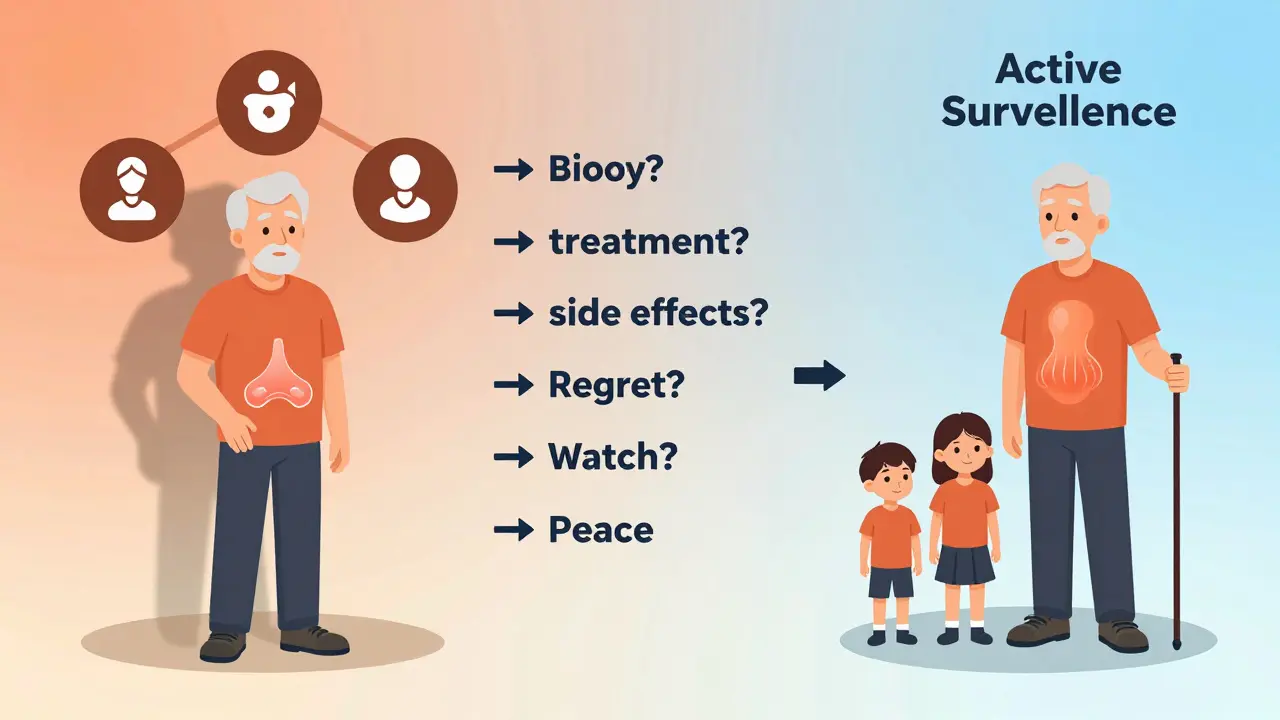
- What active surveillance is - watching the cancer with regular tests instead of jumping to surgery
Decision aids like the Ottawa Personal Decision Guide or the Mayo Clinic’s visual tool help. They show you: out of 1,000 men screened, 1 or 2 will avoid dying from prostate cancer. But 240 will have a false alarm that leads to a biopsy. And 80 will be treated for cancer that would’ve never hurt them. Seeing it like that changes everything.
Who Should Even Be Screening?
It’s not for everyone. The U.S. Preventive Services Task Force says men aged 55 to 69 should consider it - and only after a discussion. For men over 70, the harms almost always outweigh the benefits. For men under 55, routine screening isn’t recommended unless you’re at high risk.
Who’s at higher risk?
- African American men - they’re more likely to get prostate cancer and more likely to die from it
- Men with a father or brother who had prostate cancer
- Men with BRCA gene mutations
For these men, a baseline PSA at age 45 can be useful. If it’s under 1.0 ng/mL, you might not need another test for 5-10 years. If it’s higher, you might need more frequent checks or advanced testing.

What’s Next? Better Tools Are Coming
PSA isn’t the end of the story. New tests are already here. The 4Kscore test combines four proteins with your age and family history to give a clearer picture of your risk for aggressive cancer. It’s 95% accurate at ruling out high-risk disease. The PCA3 urine test looks at genetic markers in urine after a digital exam. Multiparametric MRI can scan the prostate without a needle - and studies show it cuts unnecessary biopsies by 27%.
Then there’s IsoPSA, a new version of the PSA test approved by the FDA in 2021. It doesn’t just measure total PSA - it looks at how the protein is shaped. That gives it 92% accuracy in spotting aggressive cancer, compared to just 25% for the old test. And AI tools are now analyzing routine blood work to predict cancer risk with 85% accuracy - potentially cutting down on unnecessary PSA tests by 30%.
But here’s the catch: these tests cost hundreds or even thousands of dollars. PSA costs $20 to $50. Most insurance covers it. The new ones? Often don’t. So for now, PSA remains the gateway - but it’s no longer the final word.
The Real Problem Isn’t the Test - It’s the System
Doctors are stretched thin. A 2022 study found primary care docs spend just 3.7 minutes talking about PSA screening. That’s not enough to explain risks, answer questions, or help someone make a personal decision. Only 38% of U.S. clinics have formal shared decision-making protocols. Even when they do, many doctors aren’t trained to use them.
And the disparities are stark. African American men are 23% less likely to get a real conversation about PSA screening - even though they’re twice as likely to die from prostate cancer. That’s not just a gap in care. It’s a gap in justice.
What Should You Do?
If you’re a man between 55 and 69:
- Don’t wait for your doctor to bring it up. Ask: "Should I get a PSA test?"
- Ask: "What are the chances this test will help me? What are the chances it will hurt me?"
- Ask: "What happens if my PSA is high? Do I automatically get a biopsy? Are there other tests first?"
- Ask: "If I have cancer, do I have to treat it right away? Is active surveillance an option?"
- Ask: "Do you have a decision aid I can look at?"
If you’re under 55 or over 70, ask: "Is there any reason I should be screened at all?"
If you’re African American or have a family history, ask: "Should I get a baseline PSA at 45?"
There’s no one-size-fits-all answer. But there is one rule: never let someone else decide for you. This isn’t about being scared or being brave. It’s about knowing what you’re signing up for.
It’s Not About Avoiding the Test - It’s About Choosing Wisely
PSA screening isn’t good or bad. It’s a tool. And like any tool, its value depends on how you use it. Used blindly, it causes harm. Used with understanding, it can save lives. The controversy isn’t going away. But the solution is clear: stop treating screening like a routine checkbox. Start treating it like a life decision.
Because when it comes to your body, the most powerful thing you can do isn’t to get tested. It’s to understand what the test really means - and then decide for yourself.
Is PSA screening still recommended?
Yes - but only for men aged 55 to 69, and only after a full discussion with a doctor about the risks and benefits. For men under 55 or over 70, routine screening isn’t recommended unless you’re at high risk for prostate cancer. The goal isn’t to screen everyone - it’s to help the right people make the right choice.
What’s the biggest risk of PSA screening?
The biggest risk is overdiagnosis and overtreatment. About 80 to 100 out of every 1,000 men screened will be diagnosed with prostate cancer that would never cause symptoms or harm. But once diagnosed, most men feel pressured to treat it - leading to side effects like incontinence and impotence that can last a lifetime.
Can PSA screening miss aggressive prostate cancer?
Yes. About 15% of men with aggressive, life-threatening prostate cancer have PSA levels below 4.0 ng/mL - the traditional cutoff. That means the test can give a false sense of security. That’s why some experts recommend starting with a baseline PSA at age 45, especially for high-risk men.
What are the alternatives to PSA screening?
Multiparametric MRI can scan the prostate without a biopsy and reduce unnecessary procedures by 27%. The 4Kscore test combines four blood markers with clinical data to better predict aggressive cancer risk. The PCA3 urine test looks at genetic signals after a digital exam. Genomic tests like Oncotype DX GPS can tell if a diagnosed cancer is likely to spread. But these are often expensive and not yet covered by all insurance plans.
What is active surveillance?
Active surveillance means monitoring a low-risk prostate cancer with regular PSA tests, MRIs, and biopsies - instead of jumping to surgery or radiation right away. Studies like the ProtecT trial show that after 10 years, survival rates are the same as with immediate treatment - but men on active surveillance avoid side effects like incontinence and impotence. It’s now the standard for low-risk cases.
Why are African American men at higher risk?
African American men have a 70% higher chance of getting prostate cancer and more than double the death rate compared to white men. They’re also 23% less likely to have a shared decision-making conversation before screening. This gap isn’t biological - it’s systemic. Better access to information, culturally competent care, and earlier baseline testing could close this gap.
Should I get a PSA test if I feel fine?
Prostate cancer often has no symptoms until it’s advanced. Feeling fine doesn’t mean you’re safe. But feeling fine also doesn’t mean you need a test. The key is to talk to your doctor - not because you’re sick, but because you’re making an informed choice. If you’re 55 to 69, ask: "What are the odds this test helps me versus hurts me?" That’s the only question that matters.
What if my doctor pushes me to get tested?
You have the right to say no - even if your doctor recommends it. If your doctor doesn’t explain the risks, ask for more time or a decision aid. If they dismiss your concerns, consider finding a provider who respects your right to make your own choices. Screening isn’t a medical necessity - it’s a personal decision.




Matt W
February 1, 2026 AT 22:59